Back
Poster, Podium & Video Sessions
Moderated Poster
MP20: Trauma/Reconstruction/Diversion: External Genitalia Reconstruction and Urotrauma (including transgender surgery) I
MP20-06: Perirenal Fat Thickness is Associated with Renal Trauma Injury Grade
Saturday, May 14, 2022
7:00 AM – 8:15 AM
Location: Room 225
Nizar Hakam*, Jason Lui, Nathan Shaw, Behnam Nabavizadeh, Patrick Low, Kevin Li, Benjamin Breyer, San Francisco, CA
Poster Presenter(s)
Introduction: Previous research has demonstrated an association between increased body mass index (BMI) and lower risk of high-grade renal trauma (HGRT) in patients sustaining blunt injuries. We hypothesize this association is related to a shock-absorbing effect of adiposity around the kidney. We aim to explore the association between perirenal fat thickness (PFT) and renal trauma grade. We hypothesize that patients with greater perirenal fat will have lower rates of high-grade renal injury following blunt trauma.
Methods: We identified all patients with renal trauma who arrived at the emergency department of a single trauma center between 2014 and 2020. Radiology images were reviewed to measure the PFT around the uninjured kidney due to disrupted PFT around the traumatized kidney. Patients with no available images or penetrating trauma mechanism were excluded. Logistic regression was used to assess the relation between PFT and HGRT (defined as AAST renal grade IV - V), adjusting for age, sex, and injury severity scale. Linearity assumption of PFT in the regression model was checked with restricted cubic splines analysis.
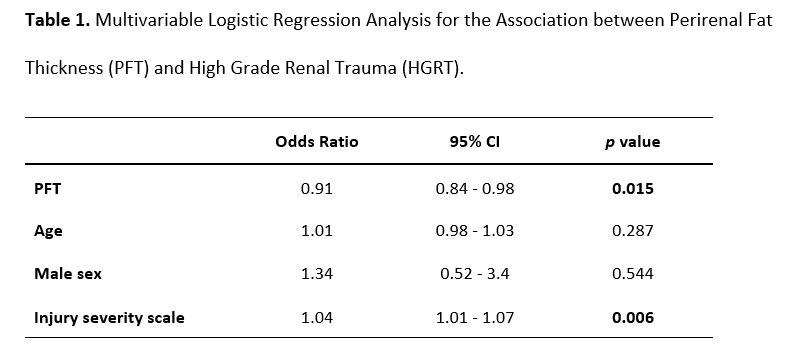
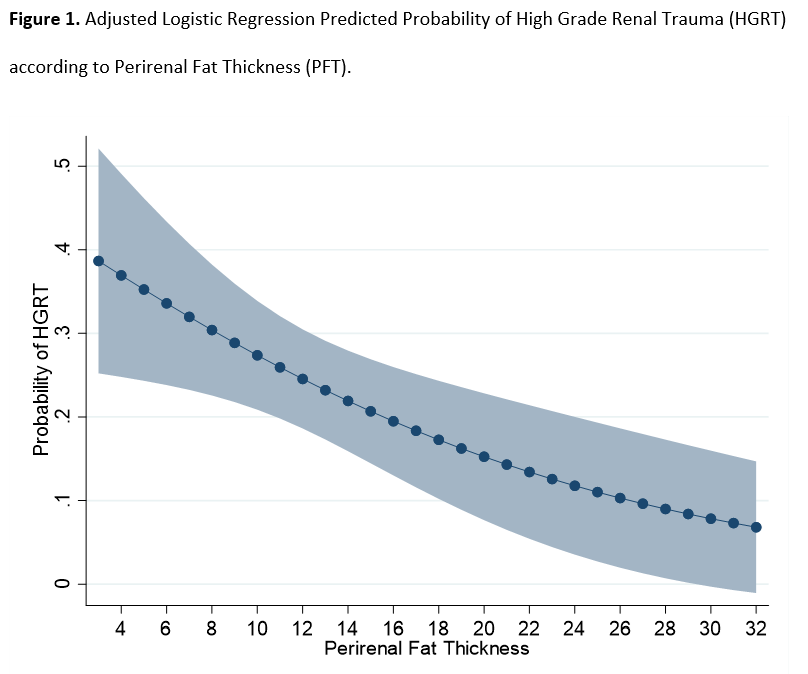
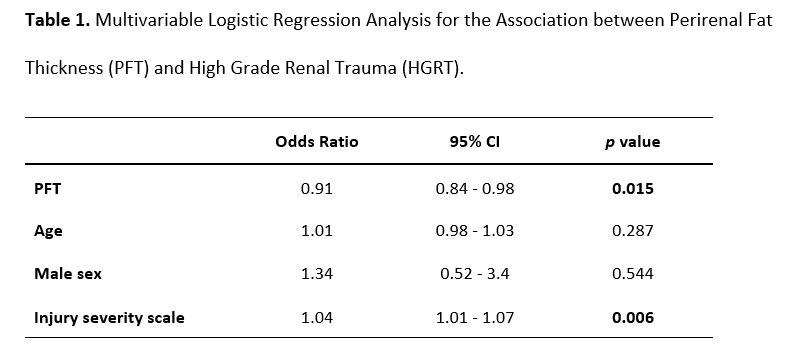
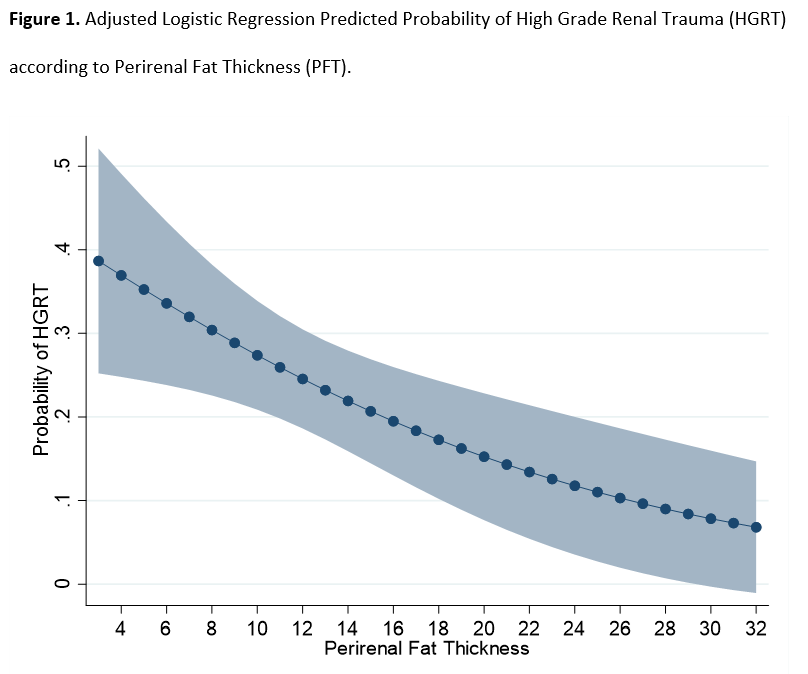
Results: 150 patients with renal trauma were included. Median age was 38.5 years (IQR 26 – 52) and 106 (70.7%) were males. PFT ranged between 2.1 and 50.1 mm, and 31 (20.7%) had HGRT. Interestingly, PFT only mildly correlates with BMI (Pearson correlation coefficient = 0.42, p < 0.0001). Those with HGRT had significantly lower PFT compared to those without HGRT (median 9.5 mm vs 11.9 mm, p = 0.047). In the multivariable analysis adjusting for age, sex, and injury severity scale, increasing PFT was associated with decreased odds (OR 0.91, 95% CI 0.84 – 0.98, p = 0.015) of HGRT (Table 1). Figure 1 depicts the model predicted probability of HGRT according to PFT.
Conclusions: Increasing perirenal fat thickness is associated with lower risk of high grade renal trauma following blunt injury. These results support a protective cushion role of adiposity in renal trauma. Notably, PFT was not strongly correlated with BMI, underscoring limitations of BMI as an accurate adiposity measure.
Source of Funding: None
Methods: We identified all patients with renal trauma who arrived at the emergency department of a single trauma center between 2014 and 2020. Radiology images were reviewed to measure the PFT around the uninjured kidney due to disrupted PFT around the traumatized kidney. Patients with no available images or penetrating trauma mechanism were excluded. Logistic regression was used to assess the relation between PFT and HGRT (defined as AAST renal grade IV - V), adjusting for age, sex, and injury severity scale. Linearity assumption of PFT in the regression model was checked with restricted cubic splines analysis.
Results: 150 patients with renal trauma were included. Median age was 38.5 years (IQR 26 – 52) and 106 (70.7%) were males. PFT ranged between 2.1 and 50.1 mm, and 31 (20.7%) had HGRT. Interestingly, PFT only mildly correlates with BMI (Pearson correlation coefficient = 0.42, p < 0.0001). Those with HGRT had significantly lower PFT compared to those without HGRT (median 9.5 mm vs 11.9 mm, p = 0.047). In the multivariable analysis adjusting for age, sex, and injury severity scale, increasing PFT was associated with decreased odds (OR 0.91, 95% CI 0.84 – 0.98, p = 0.015) of HGRT (Table 1). Figure 1 depicts the model predicted probability of HGRT according to PFT.
Conclusions: Increasing perirenal fat thickness is associated with lower risk of high grade renal trauma following blunt injury. These results support a protective cushion role of adiposity in renal trauma. Notably, PFT was not strongly correlated with BMI, underscoring limitations of BMI as an accurate adiposity measure.
Source of Funding: None

.jpg)
.jpg)
