Back
Poster, Podium & Video Sessions
Moderated Poster
MP23: Bladder Cancer: Invasive III
MP23-04: Benefit of Neoadjuvant Chemotherapy for Invasive Bladder Cancer Patients Treated with Radiation-based Therapy: An Inverse Probability Treatment Weighted Analysis
Saturday, May 14, 2022
8:45 AM – 10:00 AM
Location: Room 225
Ronald Kool*, Alice Dragomir, Montreal, Canada, Girish Kulkarni, Toronto, Canada, Gautier Marcq, Montreal, Canada, Rodney Breau, Ottawa, Canada, Michael Kim, Toronto, Canada, Ionut Busca, Hamidreza Abdi, Ottawa, Canada, Mark Dawidek, Vancouver, Canada, Michael Uy, Hamilton, Canada, Gagan Fervaha, Kingston, Canada, Nimira Alimohamed, Calgary, Canada, Jonathan Izawa, London, Canada, Claudio Jeldres, Sherbrooke, Canada, Ricardo Rendon, Halifax, Canada, Bobby Shayegan, Hamilton, Canada, Robert Siemens, Kingston, Canada, Peter Black, Vancouver, Canada, Wassim Kassouf, Montreal, Canada
.jpg)
Ronald Kool, MD
Uro-Oncologyst
McGill University
Poster Presenter(s)
Introduction: Neoadjuvant chemotherapy (NAC) is associated with improved survival for patients with muscle-invasive bladder cancer (MIBC) treated with radical cystectomy. Meanwhile, studies on the impact of NAC before curative radiation-based therapy (RT) are conflicting. We sought to study the effect of NAC on outcomes of MIBC patients treated with RT.
Methods: Retrospective study with 809 MIBC patients (cT2-4a, cN0-2) who underwent RT (=40Gy) at 10 academic centers across Canada. Clinico-pathological characteristics were assessed, and patients were stratified by NAC before RT. Using a standardized mean deviation (SMD) threshold of 0.10, NAC vs. no NAC cohorts were balanced using inverse probability weighted analysis (IPTW). Kaplan-Meier survival estimates and regression models were built to explore predictors of complete response (CR) and survival post-RT.
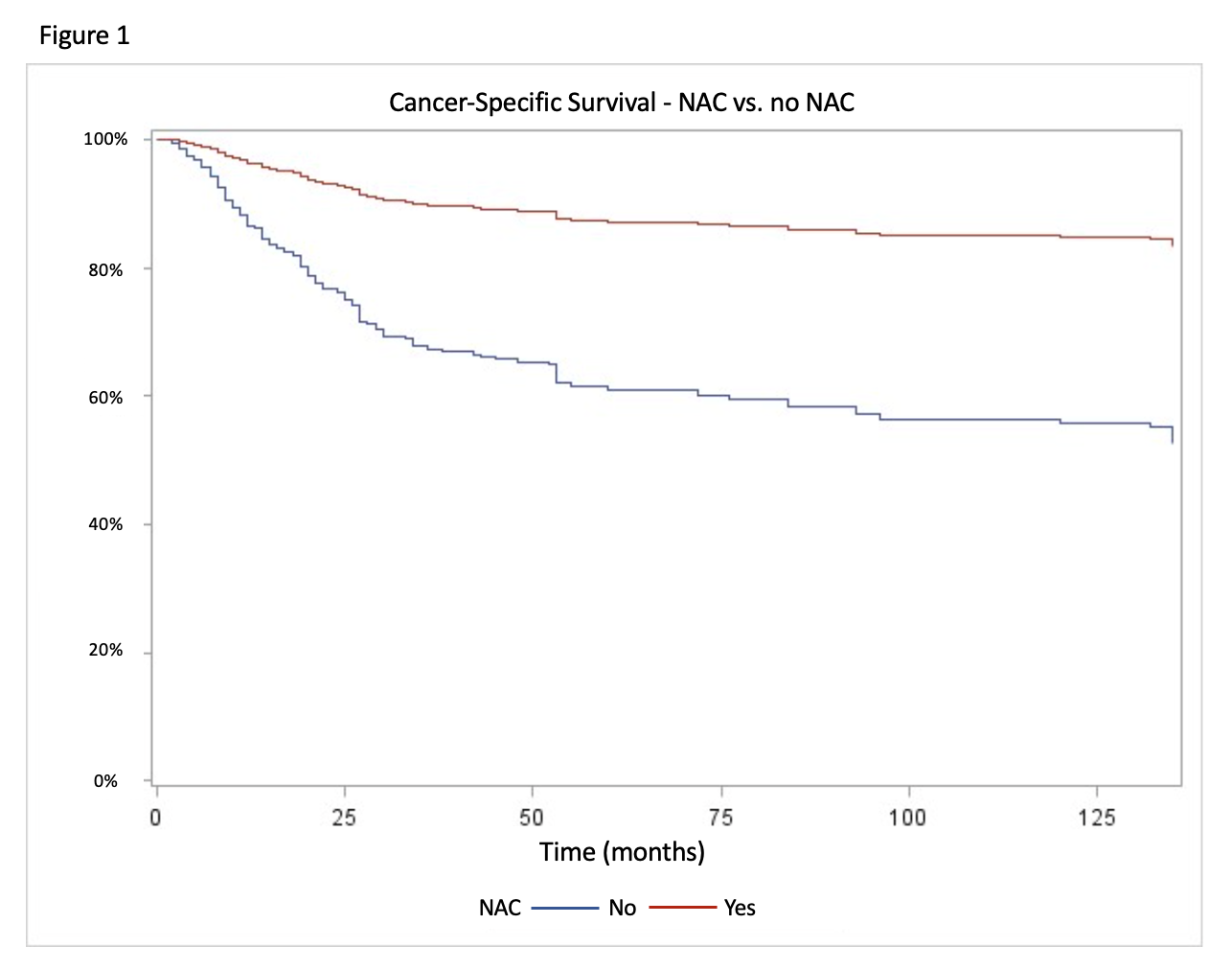
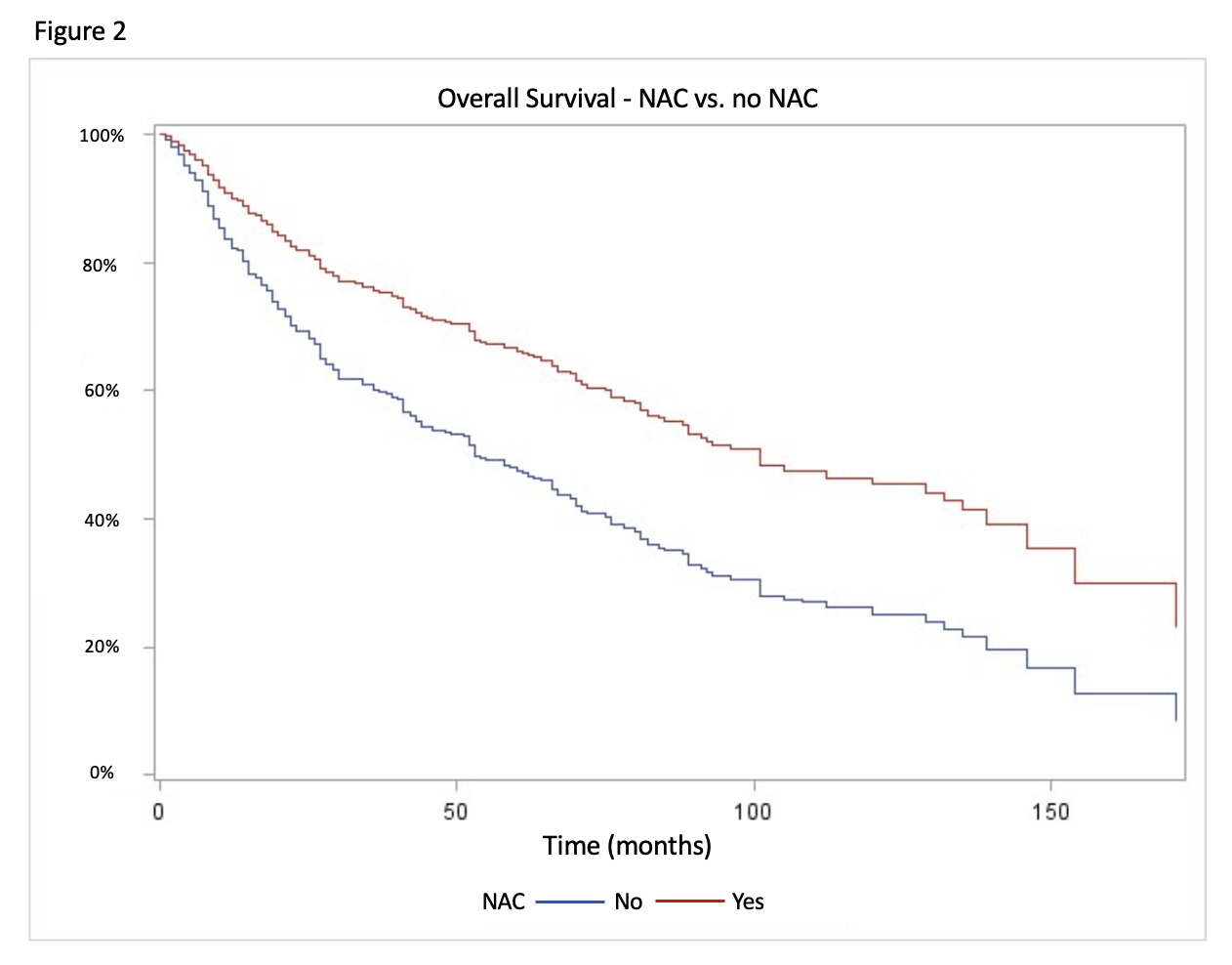
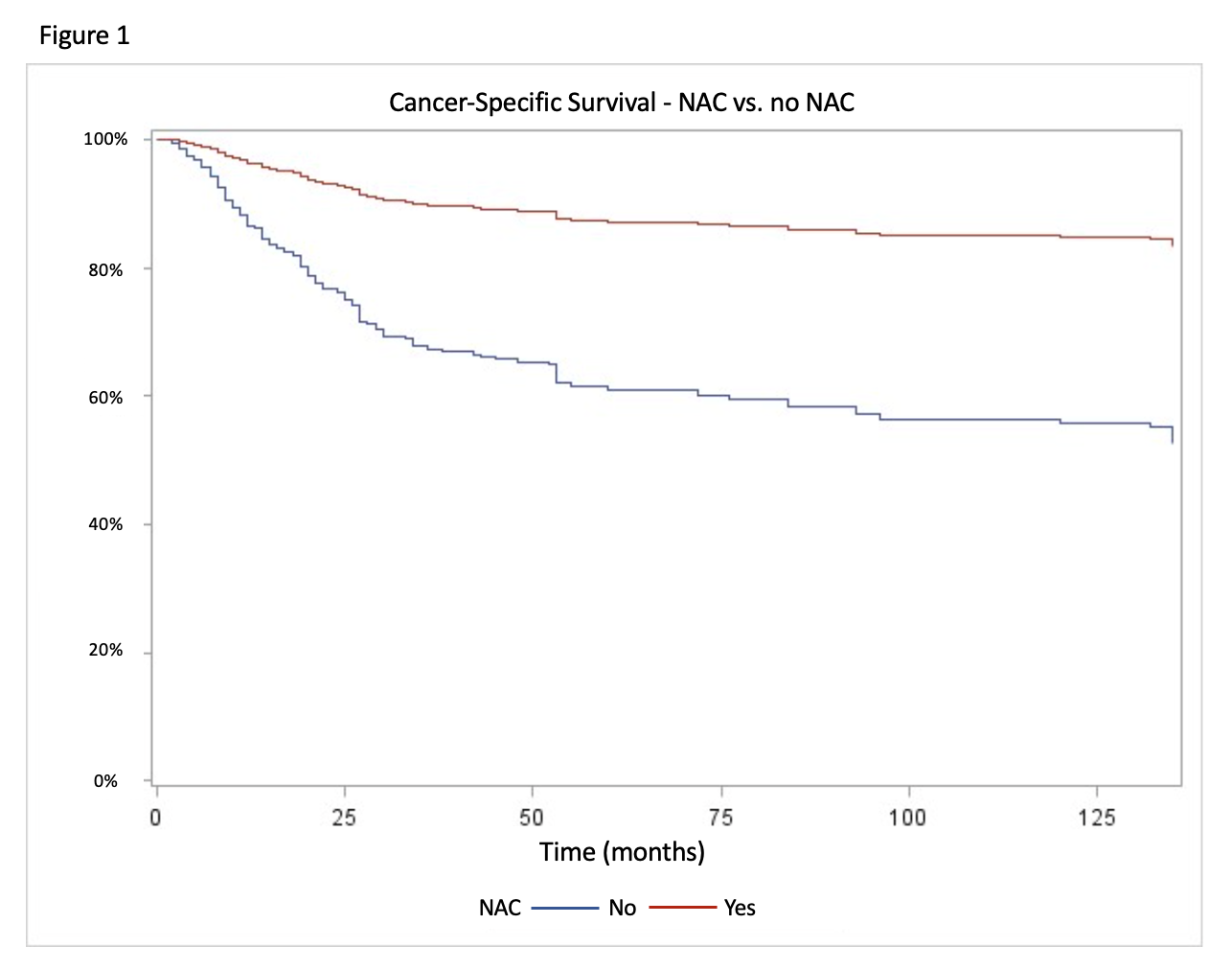
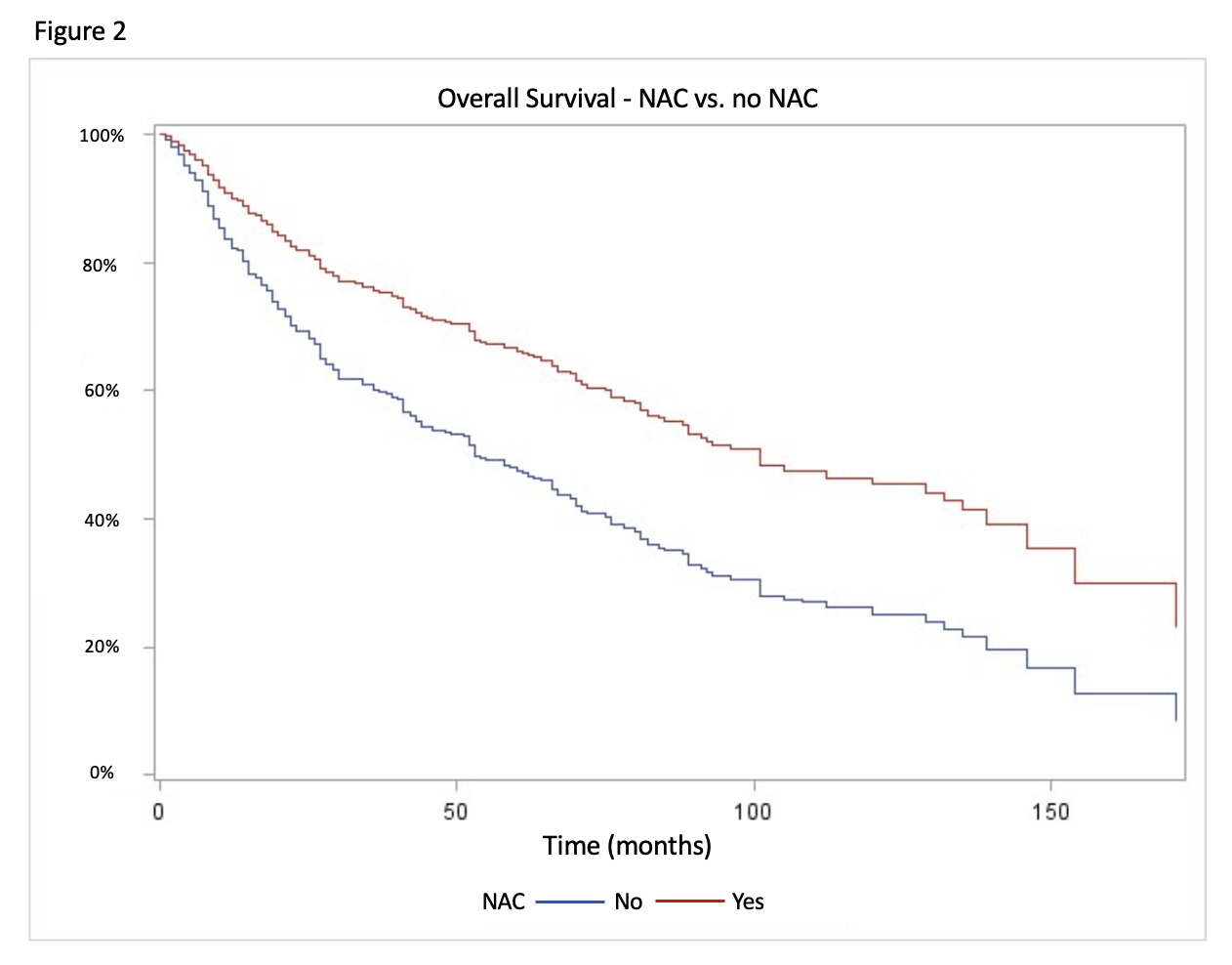
Results: Median age was 78 years [IQR 69-93], 601 (74%) patients were males, and the stage was cT2 in 641 (80%) and cN1-2 in 63 (8%) patients; 122 (15%) received NAC. In the NAC subgroup a higher proportion of patients had cN+ disease (SMD 0.27) or lymphovascular invasion (SMD 0.12) and were treated with concurrent chemotherapy (SMD 0.13) or radiation to the whole pelvis (WP-RT). After IPTW analysis, all variables were balanced between NAC vs. no NAC cohorts. Only cT stage and treatment with WP-RT were associated with CR. Multivariable analyses showed that NAC was associated with improved cancer-specific (CSS – HR 0.26; p<0.001) and overall survival (HR 0.53; p=0.003) (Fig.1 & 2), together with other prognostic factors (age, ECOG, cT stage, and WP-RT). In a subset analysis of patients treated with RT and concurrent chemotherapy, NAC remained significantly associated with CSS (HR 0.35; p=0.006).
Conclusions: In this study, NAC improved survival after RT-based therapy for MIBC. Although prospective trials are needed to validate our findings, NAC should be considered for patients planning to undergo bladder preservation with RT.
Source of Funding: None
Methods: Retrospective study with 809 MIBC patients (cT2-4a, cN0-2) who underwent RT (=40Gy) at 10 academic centers across Canada. Clinico-pathological characteristics were assessed, and patients were stratified by NAC before RT. Using a standardized mean deviation (SMD) threshold of 0.10, NAC vs. no NAC cohorts were balanced using inverse probability weighted analysis (IPTW). Kaplan-Meier survival estimates and regression models were built to explore predictors of complete response (CR) and survival post-RT.
Results: Median age was 78 years [IQR 69-93], 601 (74%) patients were males, and the stage was cT2 in 641 (80%) and cN1-2 in 63 (8%) patients; 122 (15%) received NAC. In the NAC subgroup a higher proportion of patients had cN+ disease (SMD 0.27) or lymphovascular invasion (SMD 0.12) and were treated with concurrent chemotherapy (SMD 0.13) or radiation to the whole pelvis (WP-RT). After IPTW analysis, all variables were balanced between NAC vs. no NAC cohorts. Only cT stage and treatment with WP-RT were associated with CR. Multivariable analyses showed that NAC was associated with improved cancer-specific (CSS – HR 0.26; p<0.001) and overall survival (HR 0.53; p=0.003) (Fig.1 & 2), together with other prognostic factors (age, ECOG, cT stage, and WP-RT). In a subset analysis of patients treated with RT and concurrent chemotherapy, NAC remained significantly associated with CSS (HR 0.35; p=0.006).
Conclusions: In this study, NAC improved survival after RT-based therapy for MIBC. Although prospective trials are needed to validate our findings, NAC should be considered for patients planning to undergo bladder preservation with RT.
Source of Funding: None

.jpg)
.jpg)