Back
Poster, Podium & Video Sessions
Moderated Poster
MP31: Health Services Research: Quality Improvement & Patient Safety II
MP31-08: Use of smoking cessation pharmacotherapy following cystectomy among smokers with bladder cancer
Saturday, May 14, 2022
2:45 PM – 4:00 PM
Location: Room 228
Eli Rapoport*, New York, NY, Marc Bjurlin, Chapel Hill, NC, Helena Furberg, Timothy Donahue, Bernard Bochner, Jamie Ostroff, Richard Matulewicz, New York, NY
- ER
Eli Rapoport, BS
NYU Grossman School of Medicine
Poster Presenter(s)
Introduction: Smoking is a leading cause of bladder cancer (BC). Despite the health benefits of smoking cessation following BC diagnosis, many patients continue smoking. Hospitalization for surgery may provide “teachable moments” to promote smoking cessation. We sought to assess whether evidence-based smoking cessation pharmacotherapies (SCP) were ordered for current smokers during hospitalizations following cystectomy.
Methods: The Premier Healthcare Database, an all-payer data set capturing 25% of US hospital admissions, was used to develop a sample of adult current smokers undergoing cystectomy for BC during 2009-2019. Primary outcome was receipt of SCP, defined as either nicotine replacement therapy (NRT) or prescription medications. Descriptive statistics were used to characterize the sample and the proportion of admissions where SCP was ordered. Associations between SCP and patient- and hospital-level factors were calculated using weighted and unweighted regressions, respectively. Associations between SCP order and surgical outcomes were explored using weighted logistic regressions.
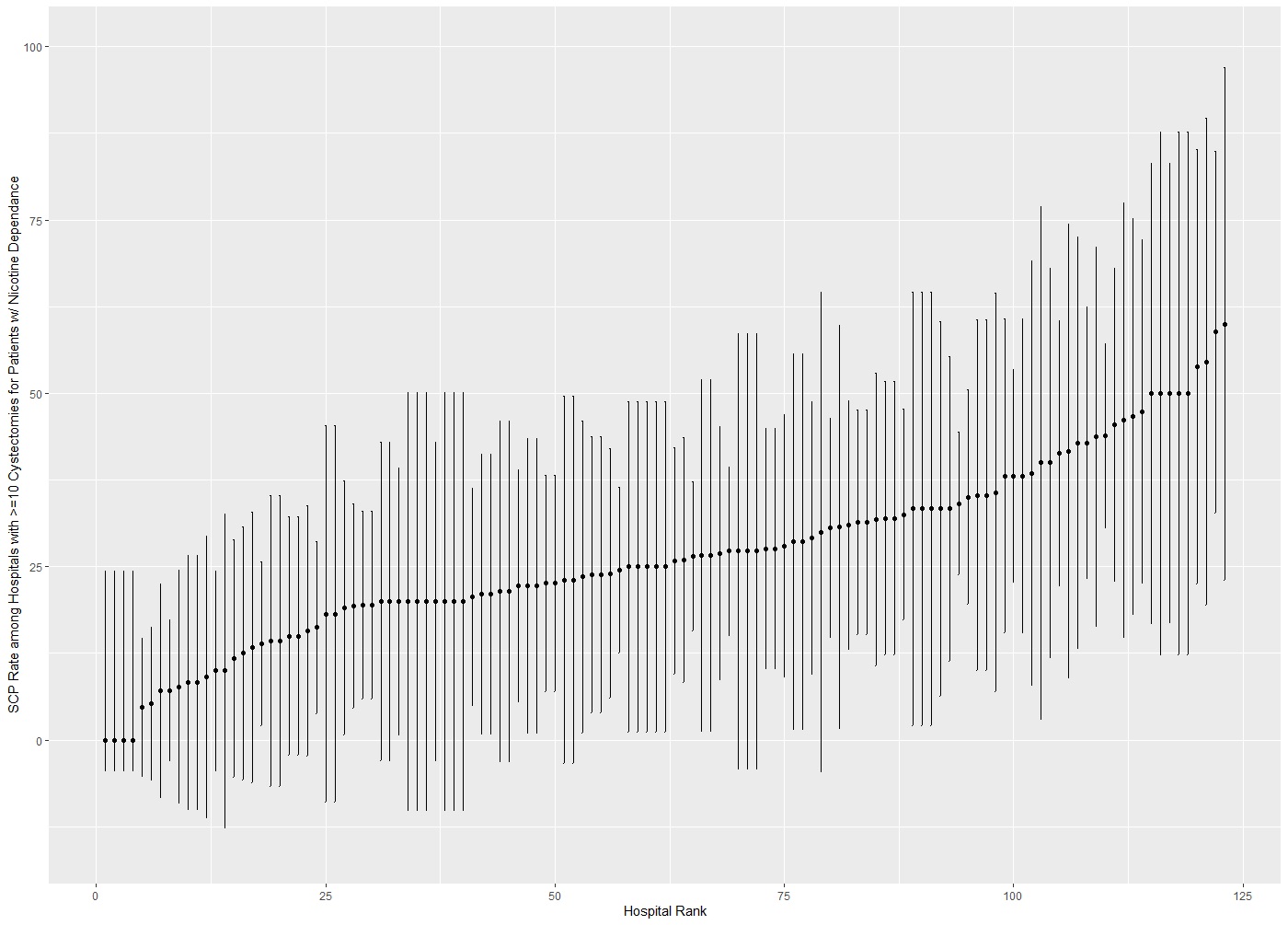
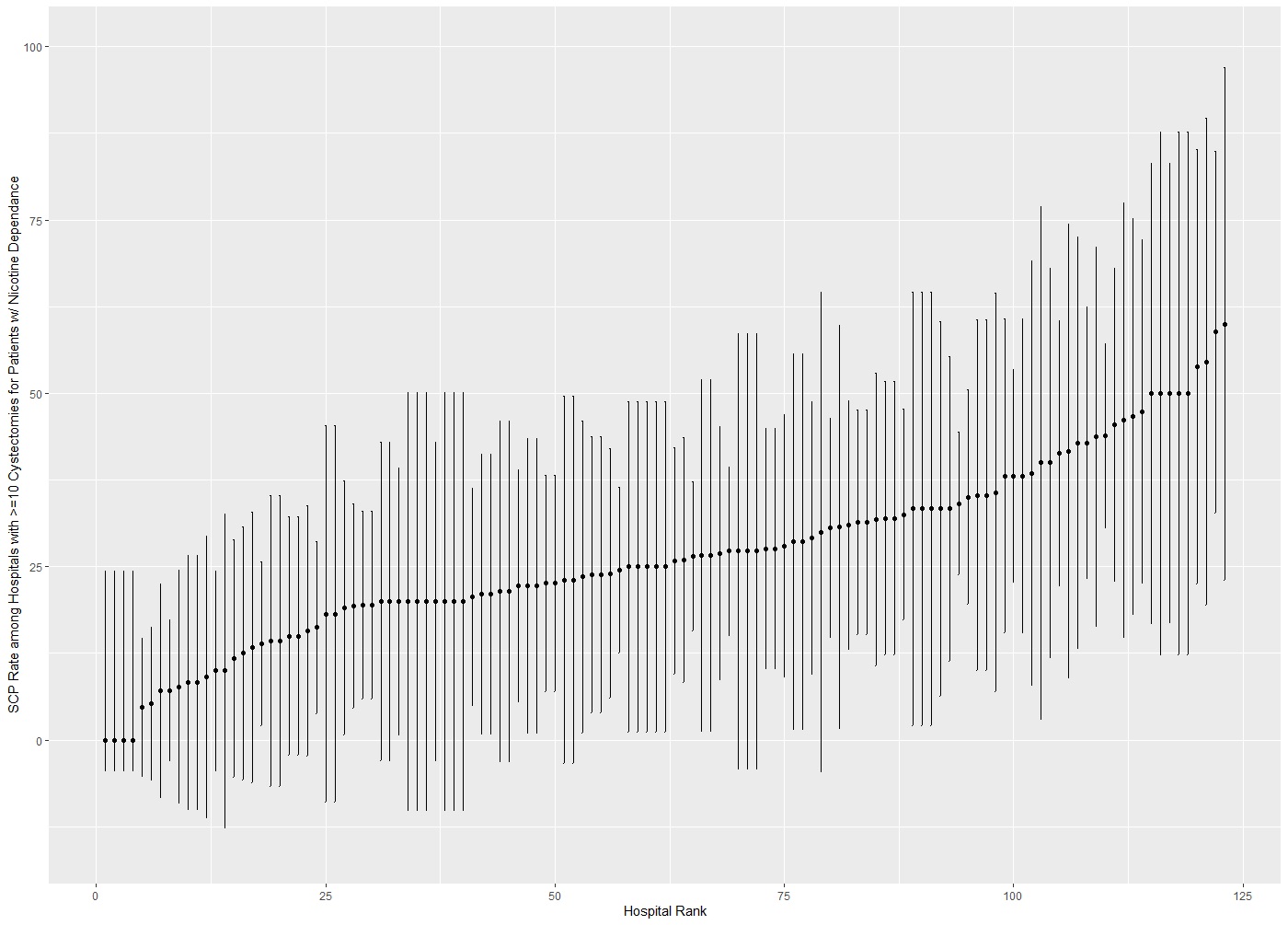
Results: In total, 3676 eligible patients (weighted N=16064) were included. Median age was 64 years, 78% were male, 7.6% Black, and the median Elixhauser comorbidity score was 10. Most patients were treated at large academic centers and underwent radical cystectomy (87.5%). 27.9% of all patients received SCP; the majority (93.6%) of orders were for NRT. At the hospital level, there was significant variation in SCP delivery (Figure). After adjustment, older and Black patients were less likely to receive SCP. Patients having radical cystectomy and those treated at Western or Midwestern (vs. Southern) hospitals were more likely to receive SCP. Patient receipt of SCP did not have a significant association with length of stay, readmission rate, or 90-day mortality after adjusting for patient factors. Hospital-level cystectomy volume did not have a significant association with receipt of SCP (adjusted ß = -0.001; 95% CI: -0.011, 0.010).
Conclusions: SCP is rarely ordered for current smokers during their inpatient admission following cystectomy. This finding demonstrates a missed opportunity to initiate evidence-based smoking cessation treatment, particularly for older and Black BC patients.
Source of Funding: none
Methods: The Premier Healthcare Database, an all-payer data set capturing 25% of US hospital admissions, was used to develop a sample of adult current smokers undergoing cystectomy for BC during 2009-2019. Primary outcome was receipt of SCP, defined as either nicotine replacement therapy (NRT) or prescription medications. Descriptive statistics were used to characterize the sample and the proportion of admissions where SCP was ordered. Associations between SCP and patient- and hospital-level factors were calculated using weighted and unweighted regressions, respectively. Associations between SCP order and surgical outcomes were explored using weighted logistic regressions.
Results: In total, 3676 eligible patients (weighted N=16064) were included. Median age was 64 years, 78% were male, 7.6% Black, and the median Elixhauser comorbidity score was 10. Most patients were treated at large academic centers and underwent radical cystectomy (87.5%). 27.9% of all patients received SCP; the majority (93.6%) of orders were for NRT. At the hospital level, there was significant variation in SCP delivery (Figure). After adjustment, older and Black patients were less likely to receive SCP. Patients having radical cystectomy and those treated at Western or Midwestern (vs. Southern) hospitals were more likely to receive SCP. Patient receipt of SCP did not have a significant association with length of stay, readmission rate, or 90-day mortality after adjusting for patient factors. Hospital-level cystectomy volume did not have a significant association with receipt of SCP (adjusted ß = -0.001; 95% CI: -0.011, 0.010).
Conclusions: SCP is rarely ordered for current smokers during their inpatient admission following cystectomy. This finding demonstrates a missed opportunity to initiate evidence-based smoking cessation treatment, particularly for older and Black BC patients.
Source of Funding: none

.jpg)
.jpg)