Back
Poster, Podium & Video Sessions
Moderated Poster
MP31: Health Services Research: Quality Improvement & Patient Safety II
MP31-10: Systematic Review and Meta-Analysis of Frailty Indices in Urologic Surgery: Risk Prediction of Postoperative Complications
Saturday, May 14, 2022
2:45 PM – 4:00 PM
Location: Room 228
Jane Kurtzman*, Preston Kerr, Rashed Kosber, Steven Brandes, New York, NY

Jane Kurtzman, MD
Columbia University Irving Medical Center
Poster Presenter(s)
Introduction: Contemporary surgical planning rarely involves formally assessing patient frailty, especially among urology (GU) patients. Our aim was to systematically review the literature to assess the ability of frailty indices to predict the risk of postoperative complications after GU surgery.
Methods: We systematically reviewed EMBASE, PubMed and SCOPUS according to PRISMA criteria in June 2021. Studies that utilized a validated frailty index (FI) to assess risk of major postoperative complication (Clavien-Dindo = 3), following GU surgery were eligible for inclusion. Charlson Comorbity Index and Eastern Cooperative Oncology Group were not considered FIs. Administrative studies, those without odds ratios (OR) and/or raw data were excluded. The pooled effect size was calculated as OR and corresponding 95% CI through a random effect model using inverse variance weighing.
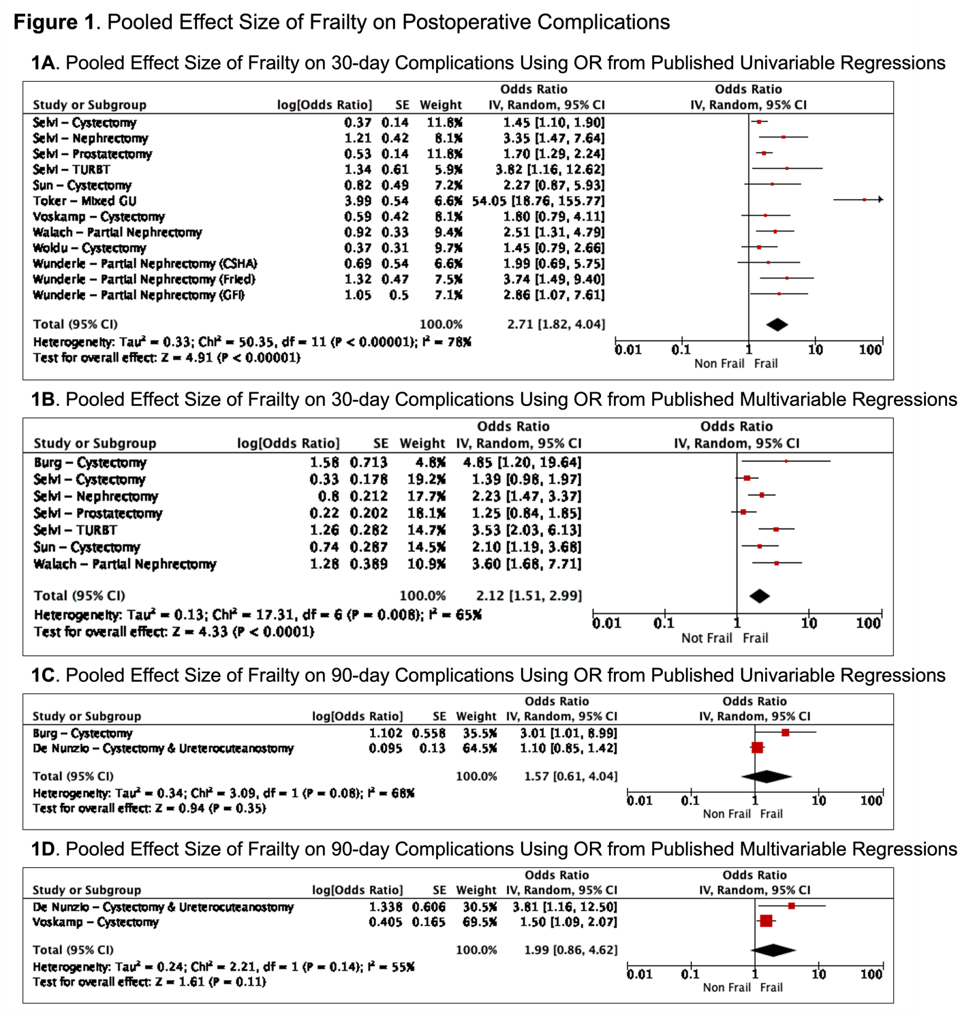
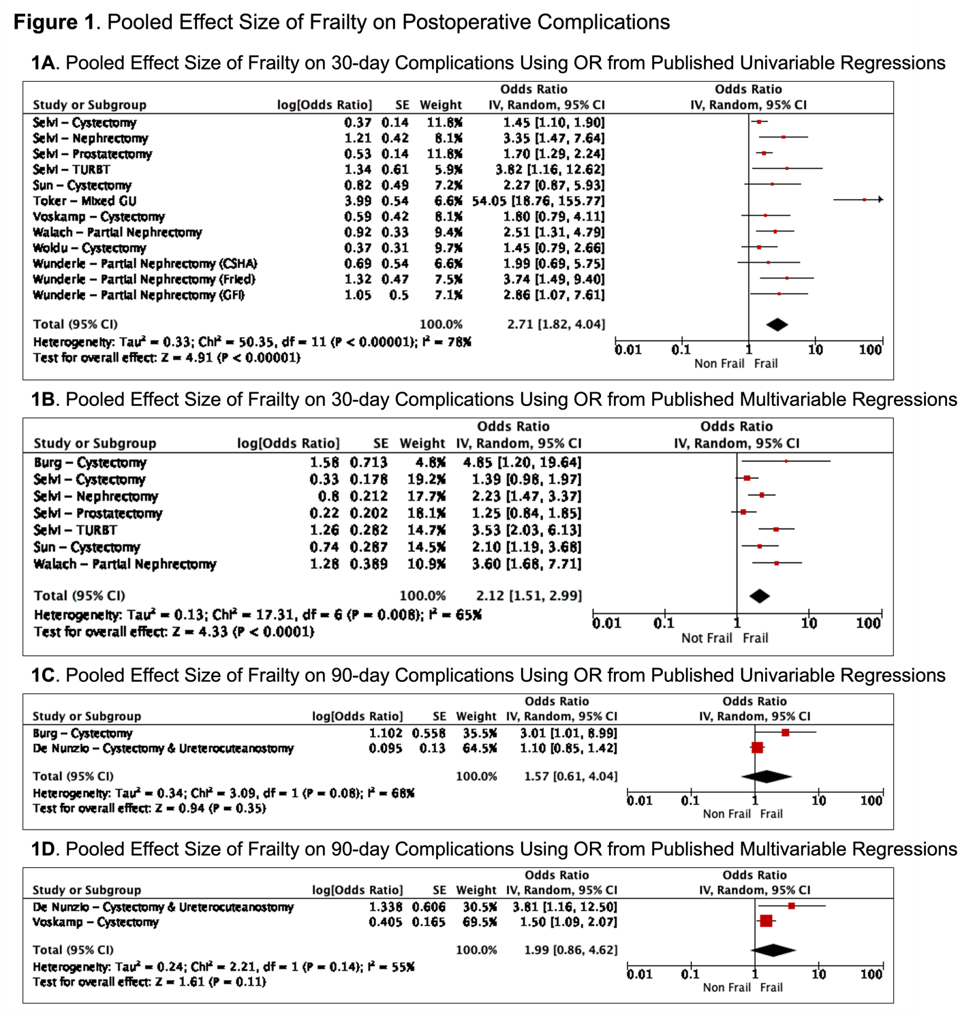
Results: Of 1,265 unique articles initially identified, 9 studies - from 6 different countries, published from 2019-2021, were eligible for inclusion (4 prospective; 5 retrospective). 8/9 studies assessed only GU oncologic surgery. The Modified Frailty Index (mFI) was the most commonly used index (n=3), followed by the Fried Phenotype Criteria (n=2), the Canadian Study of Health and Aging (CSHA) Index (n=2) and the Rockwood Frailty Index (n=2). Data from a total of 2,153 patients was included. Based on pooled OR from both univariable and multivariable analyses, frailty was associated with a significantly higher odds of postoperative complication at 30 days (OR 2.7, 95% CI: 1.8-4.0, p < 0.001 and OR 2.1, 95% CI: 1.5-3.0, p < 0.001, Fig 1A-B), but may not be at 90 days (OR 2.0, p = 0.11 and OR 1.6, p = 0.35, Fig 1C-D). Stratified by FI, higher Rockwood and CSHA scores were associated with an increased odds of 30d complication (OR 1.8, p < 0.001 and OR 2.6, p = 0.002), but mFI = 2 was not (OR 5.0, p = 0.11).
Conclusions: Frailty indices are a relatively new addition to the urologist’s toolkit. Preoperative assessment of frailty can help predict risk of early (30d) major postoperative complications but may be less useful for later complications, though significant additional studies are needed. Further work is also needed to evaluate the impact of frailty on non-oncologic urology patients who undergo major GU surgery.
Source of Funding: None
Methods: We systematically reviewed EMBASE, PubMed and SCOPUS according to PRISMA criteria in June 2021. Studies that utilized a validated frailty index (FI) to assess risk of major postoperative complication (Clavien-Dindo = 3), following GU surgery were eligible for inclusion. Charlson Comorbity Index and Eastern Cooperative Oncology Group were not considered FIs. Administrative studies, those without odds ratios (OR) and/or raw data were excluded. The pooled effect size was calculated as OR and corresponding 95% CI through a random effect model using inverse variance weighing.
Results: Of 1,265 unique articles initially identified, 9 studies - from 6 different countries, published from 2019-2021, were eligible for inclusion (4 prospective; 5 retrospective). 8/9 studies assessed only GU oncologic surgery. The Modified Frailty Index (mFI) was the most commonly used index (n=3), followed by the Fried Phenotype Criteria (n=2), the Canadian Study of Health and Aging (CSHA) Index (n=2) and the Rockwood Frailty Index (n=2). Data from a total of 2,153 patients was included. Based on pooled OR from both univariable and multivariable analyses, frailty was associated with a significantly higher odds of postoperative complication at 30 days (OR 2.7, 95% CI: 1.8-4.0, p < 0.001 and OR 2.1, 95% CI: 1.5-3.0, p < 0.001, Fig 1A-B), but may not be at 90 days (OR 2.0, p = 0.11 and OR 1.6, p = 0.35, Fig 1C-D). Stratified by FI, higher Rockwood and CSHA scores were associated with an increased odds of 30d complication (OR 1.8, p < 0.001 and OR 2.6, p = 0.002), but mFI = 2 was not (OR 5.0, p = 0.11).
Conclusions: Frailty indices are a relatively new addition to the urologist’s toolkit. Preoperative assessment of frailty can help predict risk of early (30d) major postoperative complications but may be less useful for later complications, though significant additional studies are needed. Further work is also needed to evaluate the impact of frailty on non-oncologic urology patients who undergo major GU surgery.
Source of Funding: None

.jpg)
.jpg)