Back
Poster, Podium & Video Sessions
Moderated Poster
MP43: Prostate Cancer: Localized: Active Surveillance
MP43-03: Active surveillance for low-risk prostate cancer: time trends and variation in the AUA Quality (AQUA) Registry
Sunday, May 15, 2022
10:30 AM – 11:45 AM
Location: Room 222
Matthew Cooperberg*, San Francisco, CA, William Meeks, Raymond Fang, Baltimore, MD, Franklin Gaylis, San Diego, CA, William Catalona, Chicago, IL, Danil Makarov, New York, NY

Matthew Randal Cooperberg, MD
UCSF Helen Diller Family Comprehensive Cancer Center
Poster Presenter(s)
Introduction: Active surveillance (AS) for low-risk prostate cancer is widely endorsed by major guidelines, but its use is variable as has evolved rapidly in recent years. Most extant analyses are either restricted to specific geographic regions or insurance carriers, and/or are subject to a long lag between diagnosis and data accessibility.
Methods: Data were collected from men with newly diagnosed prostate cancer in the AQUA Registry. AS was defined based on absence of active treatment and evidence of ongoing monitoring, augmented with natural language processing of physician notes. Patients were included who had known primary treatment and sufficient data to determine D’Amico risk group; those with Gleason grade group 1, PSA < 10 ng/ml, and missing T stage were included as low risk. Data from 1906 urology providers at 206 practices were included. Descriptive and summary statistics were calculated, and patterns of treatment were analyzed over time and across individual practices and providers.
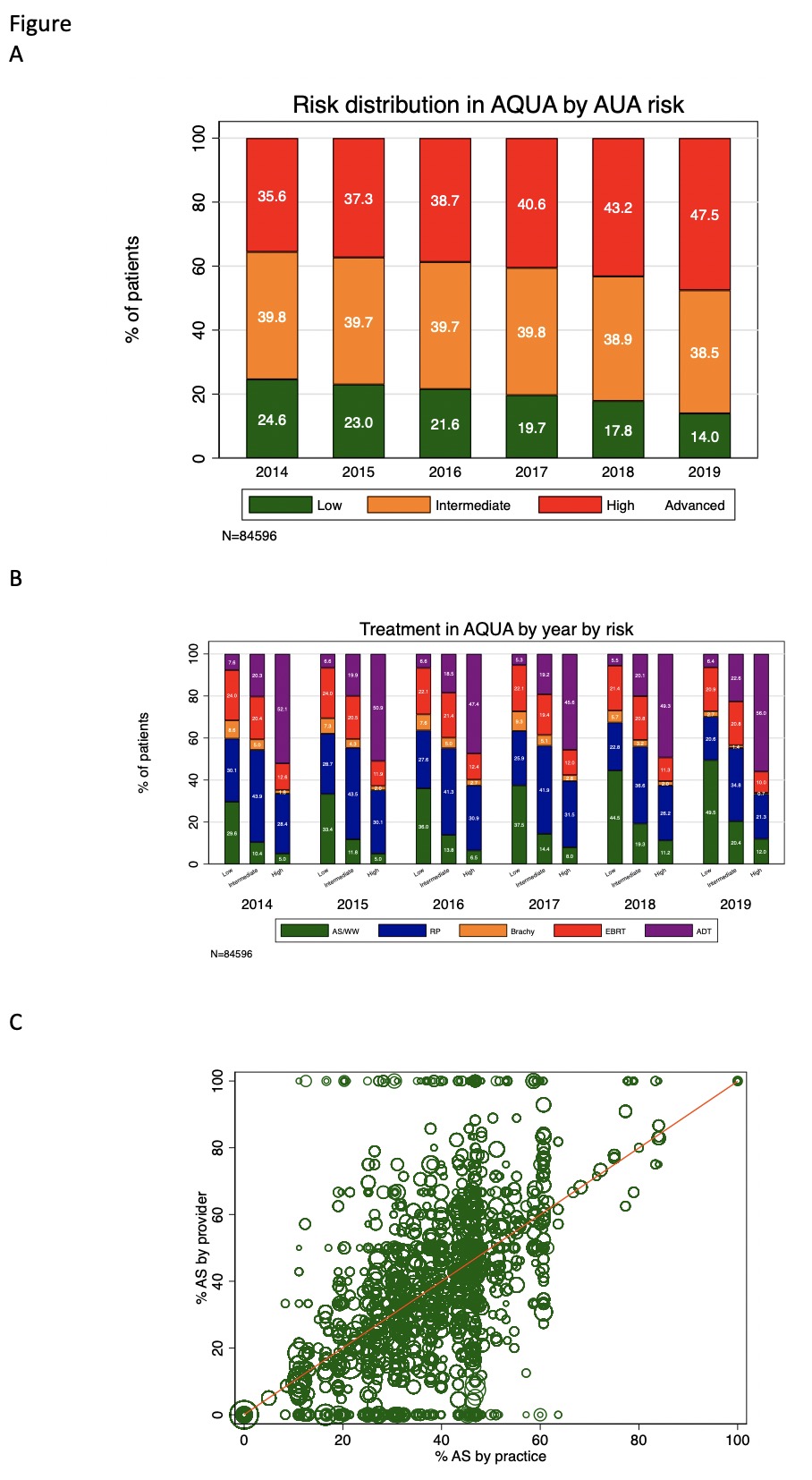
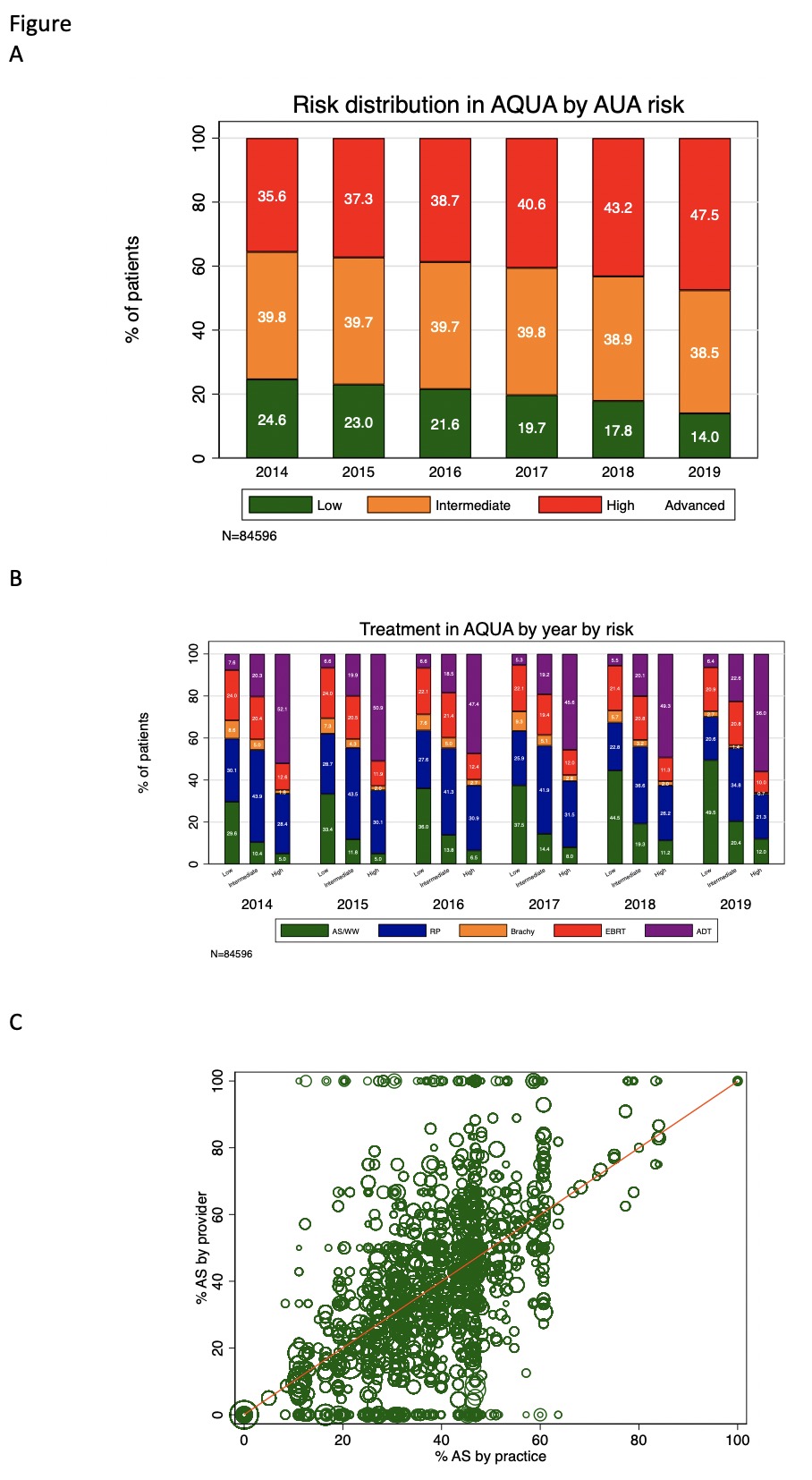
Results: From 2014 to 2019, 84,596 men in AQUA met inclusion criteria. Median (IQR) for age was 66 (61-72). Among those with known race, 79.6% were White, 15.9% Black, 1.8% Asian/Pacific Islander, 0.3% Native American, and 2.5% Other. Overall, 20.3% of men had low-risk disease at diagnosis; this proportion fell steadily from 24.6% in 2014 to 14.0% in 2019 (panel A). Across the study period, 37.1% of low- and 14.8% of intermediate-risk men chose AS as primary treatment. These figures did not vary meaningfully between White men (35.3% of low, 12.3% of intermediate risk) and Black men (34.1% of low, 12.2% of intermediate). AS rates rose over time for low-risk men from 29.6% in 2014 to 49.5% in 2019 and for intermediate-risk men from 10.4% to 20.4% (panel B). At both the practice and provider level, use of AS for men with low-risk disease ranged from 0 to 100%; provider-level AS use correlated with practice-level AS use (r=0.65, p<0.01), but with extensive provider variation within each practice (panel C).
Conclusions: AS rates for low- and intermediate-risk prostate cancer have risen sharply across the US in the past half-decade but are still suboptimal for low-risk disease in particular, and local variation is profound. Further work is needed to improve and standardize both uptake and quality of AS nationwide.
Source of Funding: AUA
Methods: Data were collected from men with newly diagnosed prostate cancer in the AQUA Registry. AS was defined based on absence of active treatment and evidence of ongoing monitoring, augmented with natural language processing of physician notes. Patients were included who had known primary treatment and sufficient data to determine D’Amico risk group; those with Gleason grade group 1, PSA < 10 ng/ml, and missing T stage were included as low risk. Data from 1906 urology providers at 206 practices were included. Descriptive and summary statistics were calculated, and patterns of treatment were analyzed over time and across individual practices and providers.
Results: From 2014 to 2019, 84,596 men in AQUA met inclusion criteria. Median (IQR) for age was 66 (61-72). Among those with known race, 79.6% were White, 15.9% Black, 1.8% Asian/Pacific Islander, 0.3% Native American, and 2.5% Other. Overall, 20.3% of men had low-risk disease at diagnosis; this proportion fell steadily from 24.6% in 2014 to 14.0% in 2019 (panel A). Across the study period, 37.1% of low- and 14.8% of intermediate-risk men chose AS as primary treatment. These figures did not vary meaningfully between White men (35.3% of low, 12.3% of intermediate risk) and Black men (34.1% of low, 12.2% of intermediate). AS rates rose over time for low-risk men from 29.6% in 2014 to 49.5% in 2019 and for intermediate-risk men from 10.4% to 20.4% (panel B). At both the practice and provider level, use of AS for men with low-risk disease ranged from 0 to 100%; provider-level AS use correlated with practice-level AS use (r=0.65, p<0.01), but with extensive provider variation within each practice (panel C).
Conclusions: AS rates for low- and intermediate-risk prostate cancer have risen sharply across the US in the past half-decade but are still suboptimal for low-risk disease in particular, and local variation is profound. Further work is needed to improve and standardize both uptake and quality of AS nationwide.
Source of Funding: AUA

.jpg)
.jpg)