Back
Poster, Podium & Video Sessions
Moderated Poster
MP43: Prostate Cancer: Localized: Active Surveillance
MP43-09: Risk of Adverse Pathology after Deferred Prostatectomy for Grade Group 1 and 2 Prostate Cancer Being Managed by Active Surveillance
Sunday, May 15, 2022
10:30 AM – 11:45 AM
Location: Room 222
Cheyenne Williams*, Philadelphia, PA, Michael Daneshvar, Patrick Gomella, Luke O'Connor, Sandeep Gurram, Peter Choyke, Bradford Wood, Baris Turkbey, Maria Merino, Peter Pinto, Bethesda, MD

Cheyenne Williams, MD
National Cancer Institute/University of Pennsylvania
Poster Presenter(s)
Introduction: There are similar pathologic and oncologic outcomes between low-risk patients on active surveillance (AS) and patients who receive immediate radical prostatectomy (RP). However, AS for patients with grade group (GG) 2 disease remains controversial. We describe pathological outcomes among patients with GG1 and GG2 prostate cancer initially managed with AS who later underwent RP and compare this to risk-matched patients who underwent immediate RP.
Methods: Patients who received RP after >1 year on AS and patients who underwent immediate RP were identified. Criteria for AS enrollment included =GG2 prostate cancer without evidence of adverse features on mpMRI. All patients received combined MRI-targeted and systematic biopsies at AS enrollment and every surveillance biopsy. Final RP pathology was then compared between NCCN risk-matched patients from each group, and multivariable logistic regression identified predictors of adverse pathology upon RP.
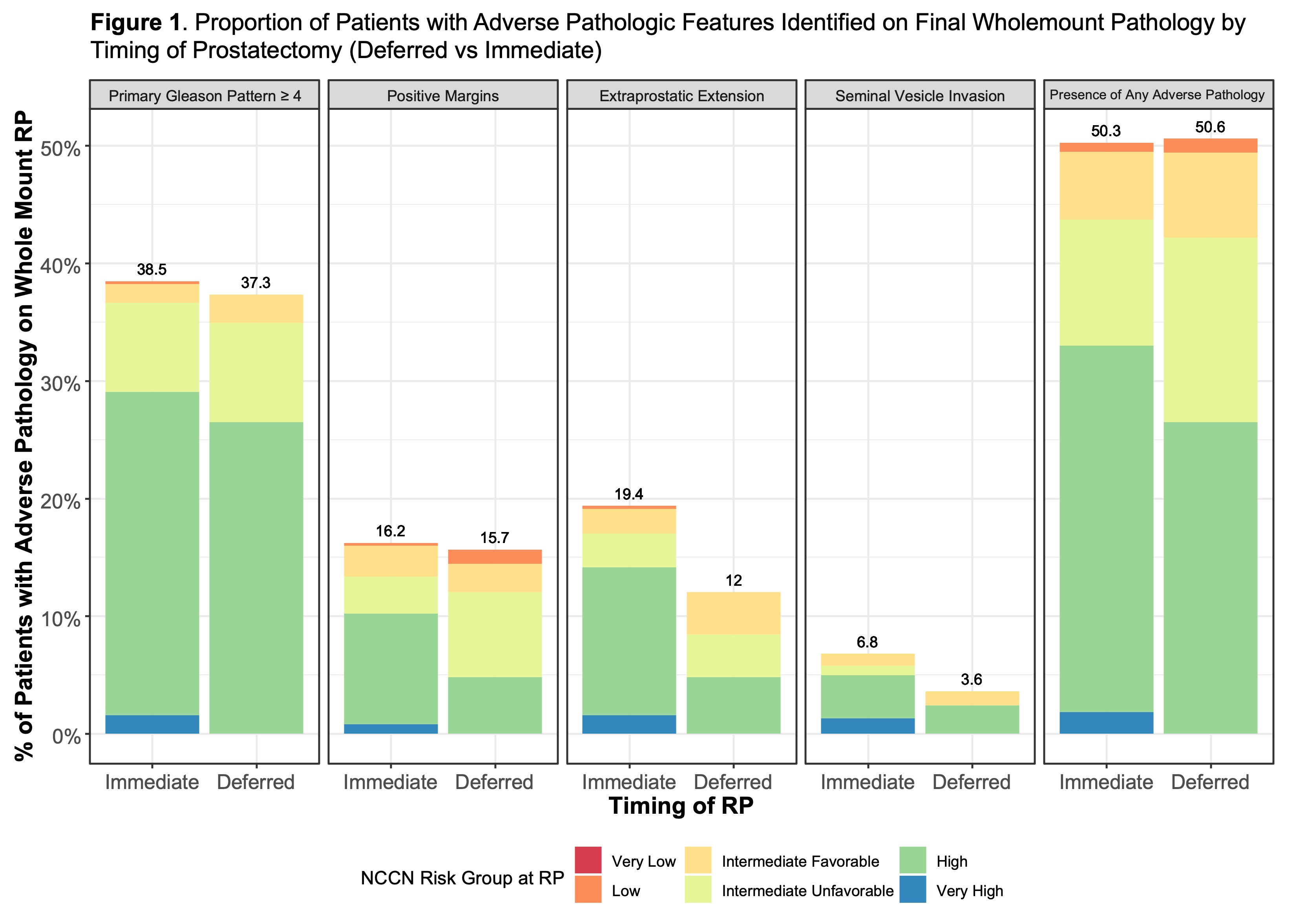
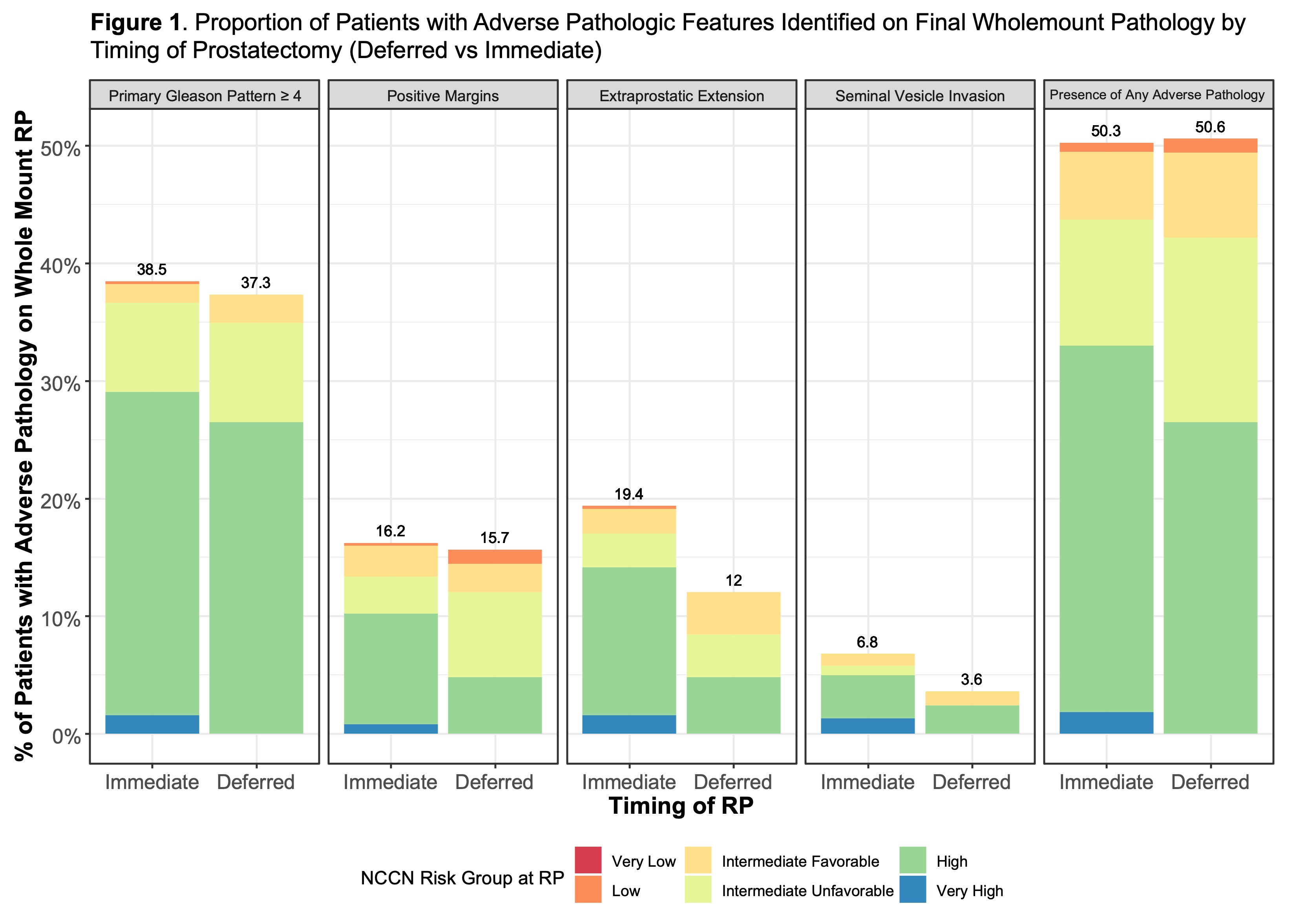
Results: 468 patients with GG1 or GG2 prostate cancer enrolled in AS at our institution, and 83 patients underwent RP after discontinuing AS. Of these, 27 (32.5%) patients were on AS with GG2 disease and 56 (67.9%) patients were on AS with GG1 disease. Median time to RP among AS patients from date of diagnosis was 39 months (IQR: 28-64). When compared to 387 risk-matched patients who underwent immediate RP (median 4 months from diagnosis), there was no difference in rates of adverse pathology for any type of adverse pathology, nor for the presence of any adverse pathology between cohorts as a whole (ps = 0.9) and when compared between NCCN risk-matched groups (Figure 1). On multivariable regression, pre-operative PSA Density (OR: 1.20 [CI: 1.04-1.42]; p<0.001) and NCCN risk group of intermediate unfavorable (OR: 3.42 [CI:1.18-12.5]; p=0.036) or high (OR: 16.8 [CI:5.71-62.3]; p<0.001) at final biopsy were independent predictors of adverse pathology. Time to RP did not predict adverse pathology.
Conclusions: In this AS cohort that included GG2 patients, patients who received deferred RP after AS had similar rates of adverse pathology compared to patients with matched risk who underwent immediate RP. Further research with longer follow-up will evaluate the oncologic and mortality outcomes of AS for GG2 disease.
Source of Funding: NIH Intramural Research Program, Foundation for NIH
Methods: Patients who received RP after >1 year on AS and patients who underwent immediate RP were identified. Criteria for AS enrollment included =GG2 prostate cancer without evidence of adverse features on mpMRI. All patients received combined MRI-targeted and systematic biopsies at AS enrollment and every surveillance biopsy. Final RP pathology was then compared between NCCN risk-matched patients from each group, and multivariable logistic regression identified predictors of adverse pathology upon RP.
Results: 468 patients with GG1 or GG2 prostate cancer enrolled in AS at our institution, and 83 patients underwent RP after discontinuing AS. Of these, 27 (32.5%) patients were on AS with GG2 disease and 56 (67.9%) patients were on AS with GG1 disease. Median time to RP among AS patients from date of diagnosis was 39 months (IQR: 28-64). When compared to 387 risk-matched patients who underwent immediate RP (median 4 months from diagnosis), there was no difference in rates of adverse pathology for any type of adverse pathology, nor for the presence of any adverse pathology between cohorts as a whole (ps = 0.9) and when compared between NCCN risk-matched groups (Figure 1). On multivariable regression, pre-operative PSA Density (OR: 1.20 [CI: 1.04-1.42]; p<0.001) and NCCN risk group of intermediate unfavorable (OR: 3.42 [CI:1.18-12.5]; p=0.036) or high (OR: 16.8 [CI:5.71-62.3]; p<0.001) at final biopsy were independent predictors of adverse pathology. Time to RP did not predict adverse pathology.
Conclusions: In this AS cohort that included GG2 patients, patients who received deferred RP after AS had similar rates of adverse pathology compared to patients with matched risk who underwent immediate RP. Further research with longer follow-up will evaluate the oncologic and mortality outcomes of AS for GG2 disease.
Source of Funding: NIH Intramural Research Program, Foundation for NIH

.jpg)
.jpg)