Back
Poster, Podium & Video Sessions
Moderated Poster
MP46: Penile & Testicular Cancer I
MP46-16: Inguinal lymph node dissection for penile cancer: results of a minimally invasive approach from a multicenter database
Sunday, May 15, 2022
1:00 PM – 2:15 PM
Location: Room 222
Aldo Brassetti*, Alfredo Bove, Umberto Anceschi, Maria Consiglia Ferriero, Salvatore Guaglianone, Riccardo Mastroianni, Leonardo Misuraca, Gabriele Tuderti, Rome, Italy, Gabriele Cozzi, Milan, Italy, Pavel Gavrilov, Barcelona, Spain, Julian Andres Chavarriaga, Bogota, Colombia, Gennaro Musi, Ottavio de Cobelli, Milan, Italy, Alberto Breda, Josep Maria Gaya Sopena, Barcelona, Spain, Diego Camacho, Rodolfo Varela, Bogota, Colombia, Giuseppe Simone, Rome, Italy

Aldo Brassetti, MD,PhD
IRCCS "Regina Elena" National Cancer Institute
Podium Presenter(s)
Introduction: open inguinal lymphadenectomy (ILND) is the gold standard for patients with invasive penile cancer (PC), dictating patient prognosis and adjuvant therapies. Due to its morbidity, minimally invasive (MI) techniques have been introduced. We describe trends in utilization and results of these novel approaches in 3 referral centers.
Methods: a purpose-built multicenter dataset was queried for patients with cM0 penile cancer (PC) treated with total/partial penectomy + lymph node dissection at the 3 participating institutions, from 2015 onwards. Baseline demographic, clinical, pathologic and perioperative data were collected. The Tetrafecta achievement [negative surgical margins (NSM), no Clavien Dindo grade =3 complications, = 7 lymph nodes (LNs) retrieved from each treated groin, no evidence of disease at 12 months (NED12mo)] was used as a proxy for surgical quality. The study population was split into 2 subgroups based on the surgical approach: categorical and continuous variables were compared using ?²- and Kruskal-Wallis tests.
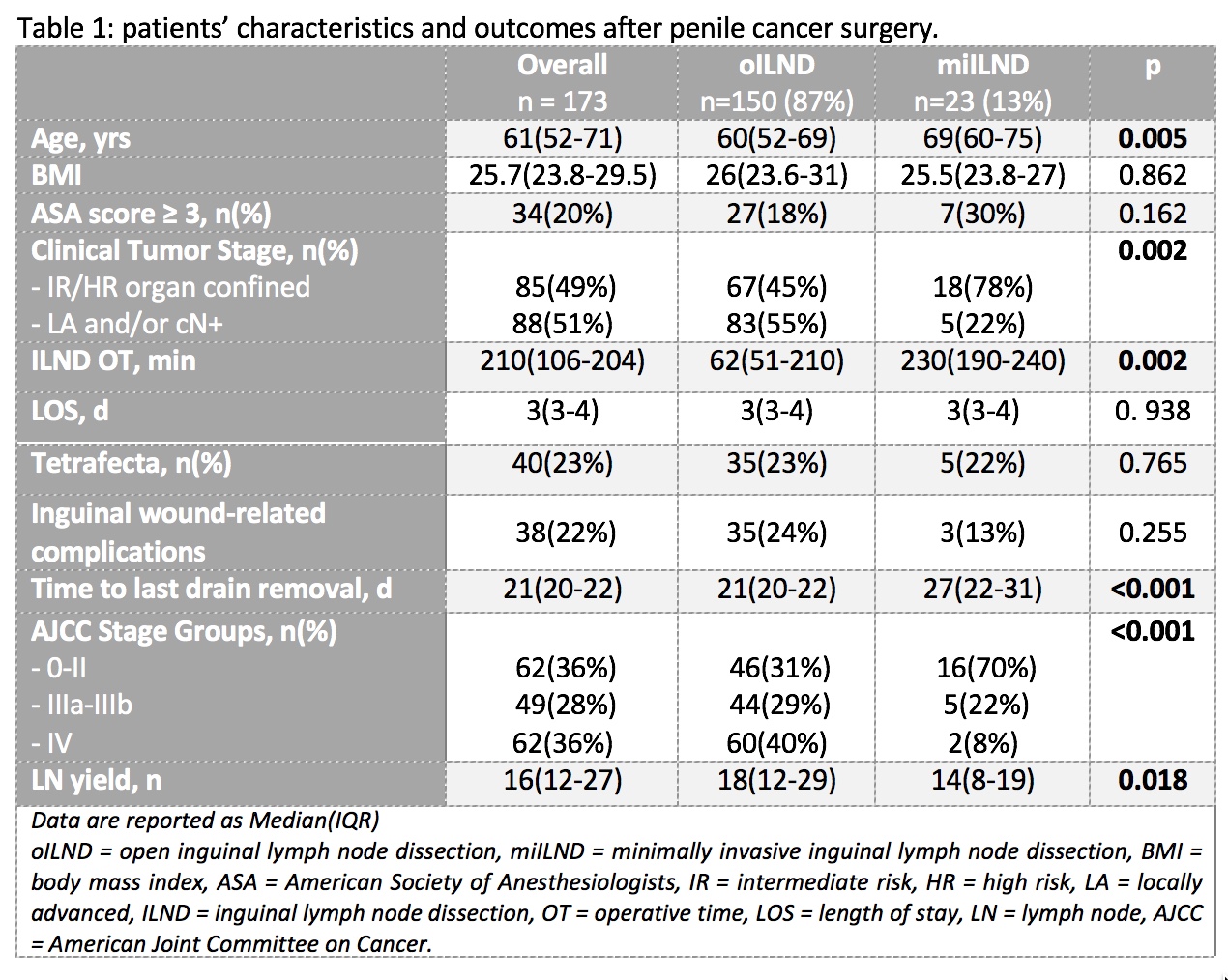
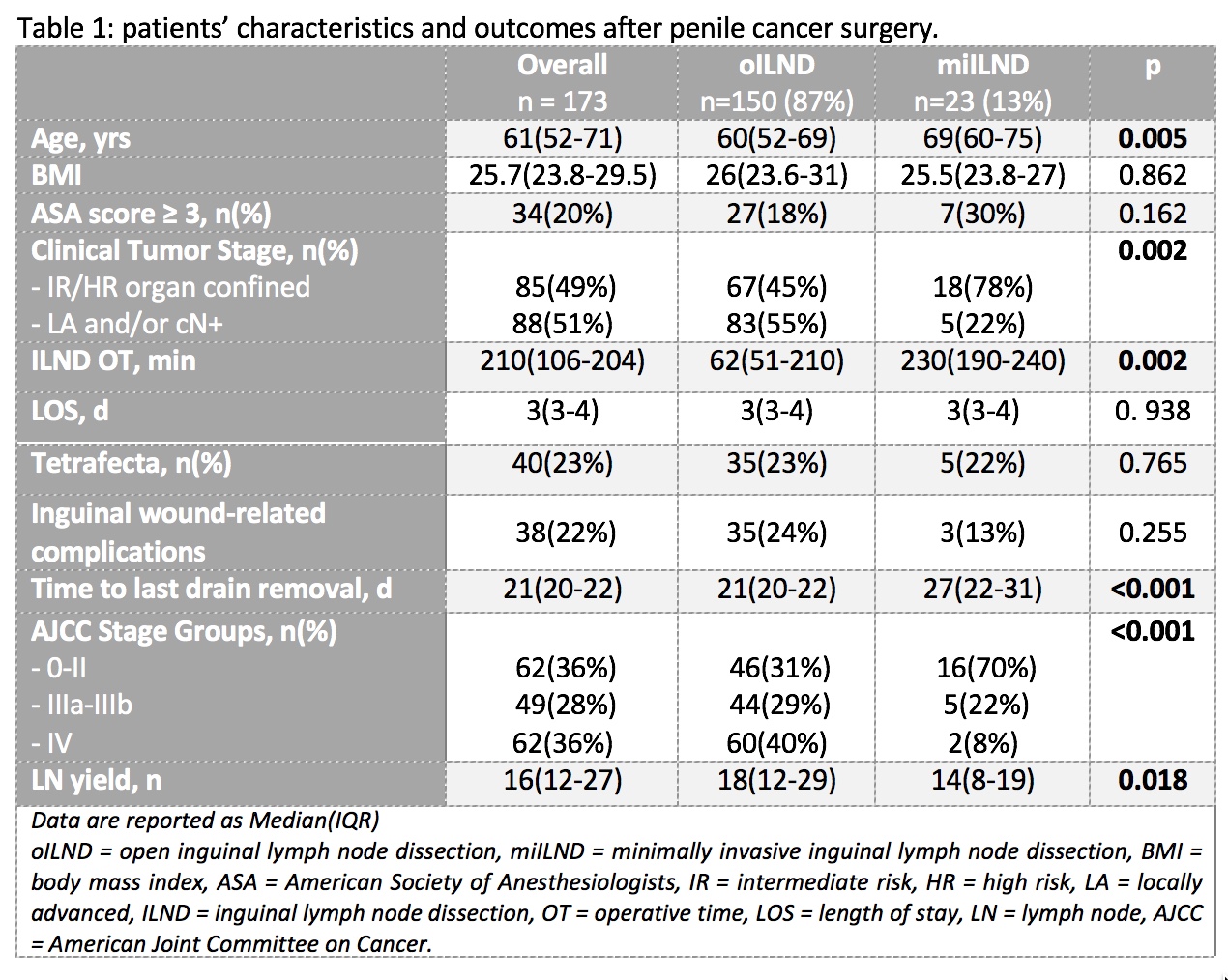
Results: overall, 173 patients were included; 23 (13%) underwent MI-ILND (Tab 1). These patients were mostly affected by tumors clinically suspected to be organ confined (78% vs 45%; p=0.002). Operation time was significantly longer in this sub-group (62 min vs 230 min; p=0.002) as the time to inguinal drains removal (21 days vs 27 days; p<0.001). Although the LN yield was significantly higher in the open cohort (p=0.018), the Tetrafecta rate was comparable in the two groups (22% vs 23%; p=0.765). Inguinal wound-related complications were less common in the MI group but the difference did not reach statistical significance (13% vs 24%; p=255).
Conclusions: MI-ILND is still underutilized although it provides surgical outcomes comparable to the open approach and may reduce wound-related complications.
Source of Funding: none
Methods: a purpose-built multicenter dataset was queried for patients with cM0 penile cancer (PC) treated with total/partial penectomy + lymph node dissection at the 3 participating institutions, from 2015 onwards. Baseline demographic, clinical, pathologic and perioperative data were collected. The Tetrafecta achievement [negative surgical margins (NSM), no Clavien Dindo grade =3 complications, = 7 lymph nodes (LNs) retrieved from each treated groin, no evidence of disease at 12 months (NED12mo)] was used as a proxy for surgical quality. The study population was split into 2 subgroups based on the surgical approach: categorical and continuous variables were compared using ?²- and Kruskal-Wallis tests.
Results: overall, 173 patients were included; 23 (13%) underwent MI-ILND (Tab 1). These patients were mostly affected by tumors clinically suspected to be organ confined (78% vs 45%; p=0.002). Operation time was significantly longer in this sub-group (62 min vs 230 min; p=0.002) as the time to inguinal drains removal (21 days vs 27 days; p<0.001). Although the LN yield was significantly higher in the open cohort (p=0.018), the Tetrafecta rate was comparable in the two groups (22% vs 23%; p=0.765). Inguinal wound-related complications were less common in the MI group but the difference did not reach statistical significance (13% vs 24%; p=255).
Conclusions: MI-ILND is still underutilized although it provides surgical outcomes comparable to the open approach and may reduce wound-related complications.
Source of Funding: none

.jpg)
.jpg)