Back
Poster, Podium & Video Sessions
Moderated Poster
MP51: Prostate Cancer: Staging
MP51-03: Development of a Novel Nomogram to Identify Candidates for Extended Pelvic Lymph-Node Dissection in Prostate Cancer using MRI and PSMA PET
Sunday, May 15, 2022
4:30 PM – 5:45 PM
Location: Room 222
Dennie Meijer*, André Vis, Amsterdam, Netherlands, Matthew Roberts, Amila Siriwardana, Andrew Morton, John Yaxley, Hemamali Samaratunga, Brisbane, Australia, Louise Emmett, Darlinghurst, Australia, Peter van de Ven, Martijn Heijmans, Henk Van der Poel, Maarten Donswijk, Thierry Boellaard, Ivo Schoots, Daniela Oprea-Lager, Amsterdam, Netherlands, Geoffrey Coughlin, Brisbane, Australia, Pim van Leeuwen, Amsterdam, Netherlands
- DM
Poster Presenter(s)
Introduction: Preoperative assessment of the probability of pelvic lymph-node metastatic (pN1) disease is required to identify patients with prostate cancer (PCa) who are candidates for extended pelvic lymph-node dissection (ePLND).
Methods: The aim of this study was to develop a novel prognostic model for predicting pathological lymph-node (pN)-status in contemporary patients with localized PCa, using preoperative clinical and histopathological parameters and imaging modalities such as magnetic resonance imaging (MRI) and prostate-specific membrane antigen (PSMA)-positron emission tomography (PET). Logistic regression with backward elimination was used to select variables for the prognostic model. Performance of the final model was evaluated using the area under the receiver operating characteristic curve (AUC) and decision-curve analyses (DCAs).
Results: Overall, 700 consecutive patients who underwent robot-assisted radical prostatectomy (RARP) and ePLND were included in the original cohort. Of these, 185/700 patients (26%) were found to have pN1-disease. The final model included initial prostate-specific antigen (PSA)-value, radiological T-stage on MRI, highest biopsy Grade Group (GG), biopsy technique (MRI-targeted versus systematic), percentage of systematic cores with clinically significant PCa (=GG2) and PSMA-PET findings. AUC for predicting pN-status was found to be 0·82 (95%CI 0·78-0·85) for the final model. The DCA demonstrated an increased net-benefit in the threshold probability =3%. Using a cut-off of 7% above which to perform ePLND, 16% of ePLNDs could have been correctly avoided. Using 10% as a cut-off to prompt ePLND, 34% of ePLNDs would be spared, in exchange of 5·5% of patients with pelvic lymph-node metastatic disease.
Conclusions: The novel nomogram to predict pelvic lymph-node metastatic disease was developed in patients with clinically localized PCa based on clinical and histopathological parameters, and parameters assessed on MRI and PSMA-PET imaging. The novel nomogram performed superior to presently available nomograms and was able to avoid ePLND in a substantial proportion of patients.
Source of Funding: None
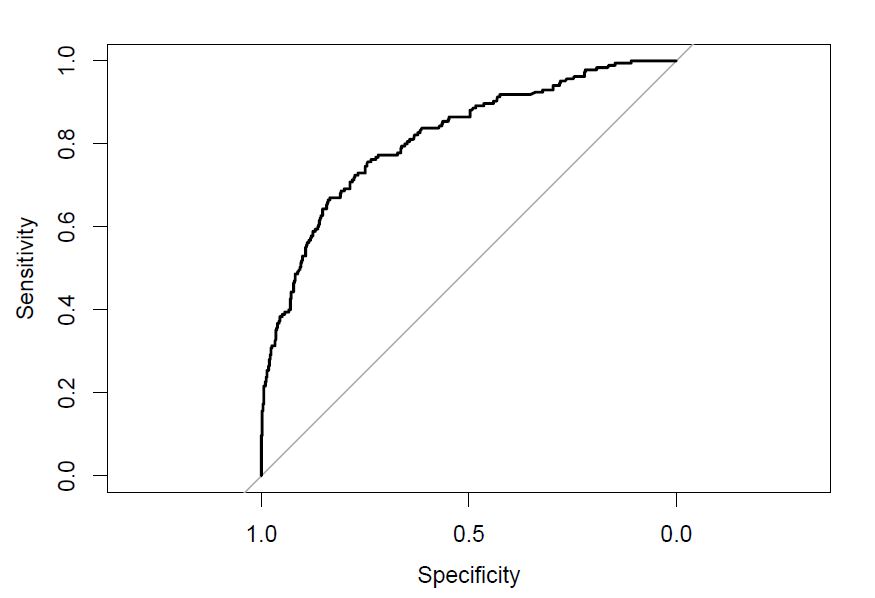
Methods: The aim of this study was to develop a novel prognostic model for predicting pathological lymph-node (pN)-status in contemporary patients with localized PCa, using preoperative clinical and histopathological parameters and imaging modalities such as magnetic resonance imaging (MRI) and prostate-specific membrane antigen (PSMA)-positron emission tomography (PET). Logistic regression with backward elimination was used to select variables for the prognostic model. Performance of the final model was evaluated using the area under the receiver operating characteristic curve (AUC) and decision-curve analyses (DCAs).
Results: Overall, 700 consecutive patients who underwent robot-assisted radical prostatectomy (RARP) and ePLND were included in the original cohort. Of these, 185/700 patients (26%) were found to have pN1-disease. The final model included initial prostate-specific antigen (PSA)-value, radiological T-stage on MRI, highest biopsy Grade Group (GG), biopsy technique (MRI-targeted versus systematic), percentage of systematic cores with clinically significant PCa (=GG2) and PSMA-PET findings. AUC for predicting pN-status was found to be 0·82 (95%CI 0·78-0·85) for the final model. The DCA demonstrated an increased net-benefit in the threshold probability =3%. Using a cut-off of 7% above which to perform ePLND, 16% of ePLNDs could have been correctly avoided. Using 10% as a cut-off to prompt ePLND, 34% of ePLNDs would be spared, in exchange of 5·5% of patients with pelvic lymph-node metastatic disease.
Conclusions: The novel nomogram to predict pelvic lymph-node metastatic disease was developed in patients with clinically localized PCa based on clinical and histopathological parameters, and parameters assessed on MRI and PSMA-PET imaging. The novel nomogram performed superior to presently available nomograms and was able to avoid ePLND in a substantial proportion of patients.
Source of Funding: None

.jpg)
.jpg)