Back
Poster, Podium & Video Sessions
Moderated Poster
MP51: Prostate Cancer: Staging
MP51-08: Does a positive multi-parametric MRI always warrant prostate biopsy? The importance of integrating clinical and imaging data based on a large, multi-institutional series.
Sunday, May 15, 2022
4:30 PM – 5:45 PM
Location: Room 222
Armando Stabile*, Giorgio Gandaglia, Elio Mazzone, Francesco Barletta, Simone Scuderi, Daniele Robesti, Giuseppe Cirulli, Donato Cannoletta, Francesco Pellegrino, Luigi Nocera, Gabriele Sorce, Mario De Angelis, Carlo Andrea Bravi, Milan, Italy, Alberto Martini, Milano, Italy, Thomas Seisen, Morgan Roupret, Paris, France - Metropolitan, Jeffrey R. Karnes, Rochester, MN, Nicola Fossati, Lugano, Switzerland, Francesco De Cobelli, Antonio Esposito, Giorgio Brembilla, Francesco Montorsi, Alberto Briganti, Milan, Italy

Armando Stabile, MD
Vita-Salute San Raffaele University
Poster Presenter(s)
Introduction: The positive predictive value (PPV) of mpMRI varies according to the risk of harbouring clinically significant prostate cancer (csPCa). However, this assumption has never been demonstrated using single patient risk data. This is key since changes in PPV is crucial to select those men who might avoid prostate biopsy despite positive imaging. We aimed at assessing the variation in PPV of mpMRI according to each patient clinical profile.
Methods: Overall, 1,945 patients with positive mpMRI (PI-RADS=3) receiving targeted (TBx) plus systematic prostate biopsy (SBx) at three tertiary centres between 2013 and 2020 were identified. The relationship between the PPV for csPCa (i.e., Gleason score=3+4) of mpMRI and individual patient risk based on clinical factors (namely, age, PSA, DRE, prostate volume, and biopsy history) was assessed. A multivariable logistic regression analysis (MVA) estimated individual patient risk of csPCa. A second MVA tested the association between individual patient risk and PPV of mpMRI. A non-parametric loess analysis graphically explored the variation in PPV of mpMRI according to clinical risk of csPCa after stratifying for PI-RADS score.
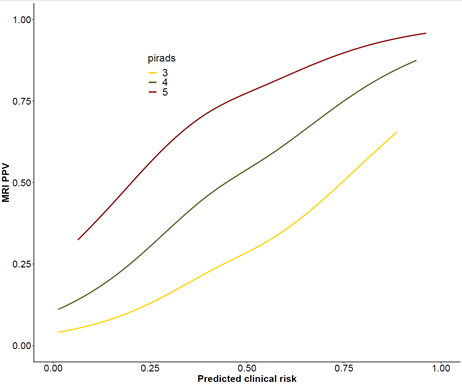
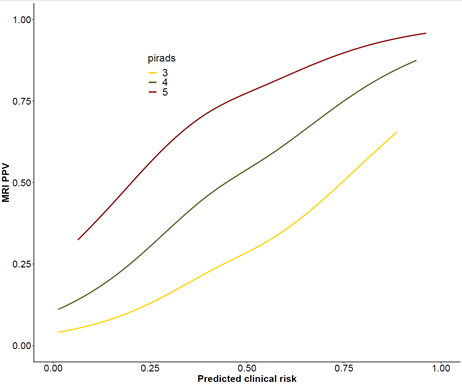
Results: Median number of TBx and SBX cores was 5 and 12, respectively. Overall, 69% and 41% of men had PCa and csPCa found at TBx and 34%, 46% and 20% of men had PI-RADS 3, 4, and 5 at mpMRI, respectively. At MVA individual patient clinical risk of harbouring csPCa was associated with PPV of mpMRI (OR: 1.4; p<0.001). Figure 1 shows that, for patients with a 5% clinical risk of csPCa vs patients with a risk higher than 90%, PPV of PI-RADS 3, 4 and 5 changed from 5% to 62%, from 13% to 80% and from 30% to 95%.
Conclusions: Individual patient clinical risk for csPCa influenced PPV of mpMRI. In men with PI-RADS 4 lesions but very low risk of csPCa based on clinical parameters, only 1 out of 10 patients had csPCa at biopsy. Based on detailed analyses of PPV, MRI should not be considered as stand-alone test triage test but rather integrated in clinical prediction models to select those men who could safely avoid prostate biopsy despite positive imaging.
Source of Funding: None.
Methods: Overall, 1,945 patients with positive mpMRI (PI-RADS=3) receiving targeted (TBx) plus systematic prostate biopsy (SBx) at three tertiary centres between 2013 and 2020 were identified. The relationship between the PPV for csPCa (i.e., Gleason score=3+4) of mpMRI and individual patient risk based on clinical factors (namely, age, PSA, DRE, prostate volume, and biopsy history) was assessed. A multivariable logistic regression analysis (MVA) estimated individual patient risk of csPCa. A second MVA tested the association between individual patient risk and PPV of mpMRI. A non-parametric loess analysis graphically explored the variation in PPV of mpMRI according to clinical risk of csPCa after stratifying for PI-RADS score.
Results: Median number of TBx and SBX cores was 5 and 12, respectively. Overall, 69% and 41% of men had PCa and csPCa found at TBx and 34%, 46% and 20% of men had PI-RADS 3, 4, and 5 at mpMRI, respectively. At MVA individual patient clinical risk of harbouring csPCa was associated with PPV of mpMRI (OR: 1.4; p<0.001). Figure 1 shows that, for patients with a 5% clinical risk of csPCa vs patients with a risk higher than 90%, PPV of PI-RADS 3, 4 and 5 changed from 5% to 62%, from 13% to 80% and from 30% to 95%.
Conclusions: Individual patient clinical risk for csPCa influenced PPV of mpMRI. In men with PI-RADS 4 lesions but very low risk of csPCa based on clinical parameters, only 1 out of 10 patients had csPCa at biopsy. Based on detailed analyses of PPV, MRI should not be considered as stand-alone test triage test but rather integrated in clinical prediction models to select those men who could safely avoid prostate biopsy despite positive imaging.
Source of Funding: None.

.jpg)
.jpg)