Back
Poster, Podium & Video Sessions
Moderated Poster
MP51: Prostate Cancer: Staging
MP51-11: Has the introduction of mpMRI in the diagnostic pathway of prostate cancer led to improved oncological outcomes after radical prostatectomy? Result from a large single-institutional series.
Sunday, May 15, 2022
4:30 PM – 5:45 PM
Location: Room 222
Armando Stabile*, Elio Mazzone, Gabriele Sorce, Francesco Barletta, Luigi Nocera, Vito Cucchiara, Milan, Italy, Emanuele Zaffuto, Federico Dehò, Varese, Italy, Donato Cannoletta, Mario De Angelis, Simone Scuderi, Giorgio Gandaglia, Milan, Italy, Giuseppe Rosiello, Antony Pellegrino, Milano, Italy, Nicola Fossati, Lugano, Switzerland, Nazareno Suardi, Genoa, Italy, Francesco De Cobelli, Antonio Esposito, Giorgio Brembilla, Milan, Italy, Shahrokh Shariat, Vienna, Austria, Francesco Montorsi, Alberto Briganti, Milan, Italy

Armando Stabile, MD
Vita-Salute San Raffaele University
Poster Presenter(s)
Introduction: The introduction of multiparametric magnetic resonance imaging (mpMRI) increased the detection of clinically significant prostate cancer (PCa). However, it is currently unknown whether mp-MRI has also led to improved cancer control. We aimed at assessing the relationship between mpMRI introduction and the rate of biochemical recurrence (BCR) after radical prostatectomy (RP) for PCa.
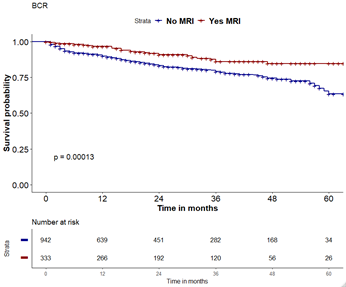
Methods: We identified 1,624 men who underwent RP at a single referral center between 2016 and 2021. Among these we identified 338 men that received an upfront mpMRI for diagnostic purposes. We assessed the impact of mpMRI for diagnostic purposes on BCR-free survival rate after RP across the two populations (MRI [n=338] vs no MRI cohort [n=1286]). BCR was defined as two PSA =0.2 ng/ml after RP. Kaplan-Meier analyses adjusted on multivariable Cox regression models (MVA) were used. Covariates were PSA, ISUP grade, pT stage, and lymph-node invasion (LNI).
Results: Median age and median PSA were 65 yrs (IQR: 59-70) and 66 yrs (IQR: 61-70) and 7.2 and 6.7 in the no MRI cohort and MRI, respectively (p=0.3). The rate of ISUP grade 1-2, 3 and 4-5 were 56%, 20%, and 18% vs 49%, 24%, and 27%, in no MRI vs MRI cohort, respectively (p>0.05). Similarly, clinical stage distribution did not differ between the two groups (p=0.1). At MVA, the use of mpMRI (HR: 0.8), PSA, ISUP grade > 2, pathological T stage > T1, and LNI, were predictor of BCR (p <0.02). The use of mpMRI for diagnostic purposes was associated with higher BCR-free survival after RP as compared to the no MRI cohort (p < 0.001).
Conclusions: The introduction of mpMRI within the diagnostic pathway of PCa is associated with an higher BCR-free survival rates. These results support the impact of mp-MRI not only as diagnostic triage test but also a beneficial tool for earlier diagnosis and thus better post-treatment outcomes.
Source of Funding: None.
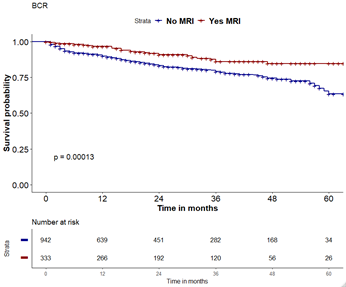
Methods: We identified 1,624 men who underwent RP at a single referral center between 2016 and 2021. Among these we identified 338 men that received an upfront mpMRI for diagnostic purposes. We assessed the impact of mpMRI for diagnostic purposes on BCR-free survival rate after RP across the two populations (MRI [n=338] vs no MRI cohort [n=1286]). BCR was defined as two PSA =0.2 ng/ml after RP. Kaplan-Meier analyses adjusted on multivariable Cox regression models (MVA) were used. Covariates were PSA, ISUP grade, pT stage, and lymph-node invasion (LNI).
Results: Median age and median PSA were 65 yrs (IQR: 59-70) and 66 yrs (IQR: 61-70) and 7.2 and 6.7 in the no MRI cohort and MRI, respectively (p=0.3). The rate of ISUP grade 1-2, 3 and 4-5 were 56%, 20%, and 18% vs 49%, 24%, and 27%, in no MRI vs MRI cohort, respectively (p>0.05). Similarly, clinical stage distribution did not differ between the two groups (p=0.1). At MVA, the use of mpMRI (HR: 0.8), PSA, ISUP grade > 2, pathological T stage > T1, and LNI, were predictor of BCR (p <0.02). The use of mpMRI for diagnostic purposes was associated with higher BCR-free survival after RP as compared to the no MRI cohort (p < 0.001).
Conclusions: The introduction of mpMRI within the diagnostic pathway of PCa is associated with an higher BCR-free survival rates. These results support the impact of mp-MRI not only as diagnostic triage test but also a beneficial tool for earlier diagnosis and thus better post-treatment outcomes.
Source of Funding: None.

.jpg)
.jpg)