Back
Poster, Podium & Video Sessions
Moderated Poster
MP52: Urodynamics/Lower Urinary Tract Dysfunction/Female Pelvic Medicine: Male Incontinence: Therapy
MP52-06: Longitudinal changes in lower urinary tract symptoms after artificial urethral sphincter implantation in patients undergoing prior radiotherapy
Monday, May 16, 2022
7:00 AM – 8:15 AM
Location: Room 228
Minato Yokoyama*, Madoka Kataoka, Yusuke Uchida, Yuki Nakamura, Shohei Fukuda, Sho Uehara, Hajime Tanaka, Soichiro Yoshida, Yoh Matsuoka, Yasuhisa Fujii, Tokyo, Japan
- MY
Minato Yokoyama, MD
Tokyo Medical and Dental University
Poster Presenter(s)
Introduction: Impact of prior radiotherapy (RT) on outcomes of artificial urinary sphincter (AUS) implantation is still controversial. Here, we evaluated longitudinal changes in lower urinary tract symptoms (LUTS) after AUS implantation in patients undergoing RT in comparison to those in non-irradiated patients.
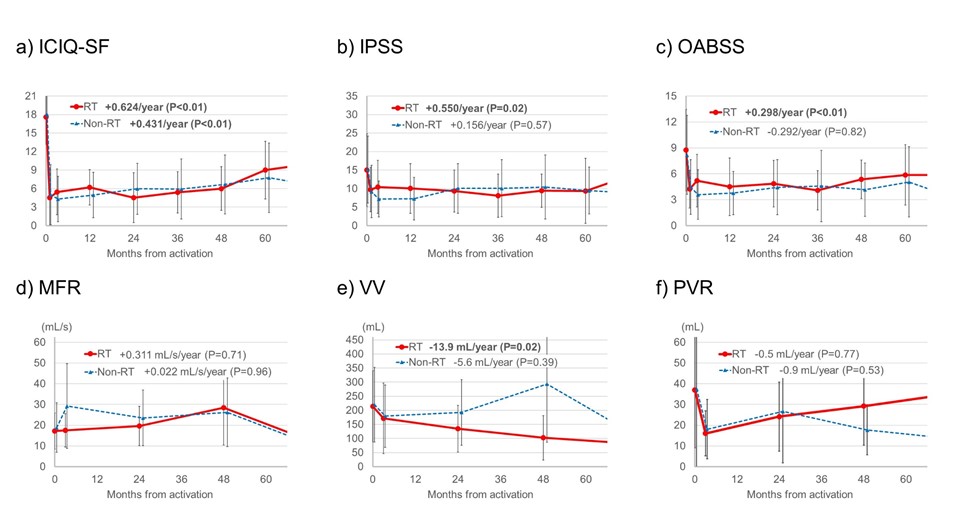
Methods: The current study included 76 patients receiving initial AUS implantation between 2010 and 2020. In principle, the patients were followed 1, 3, and 12 months after activation of the implanted AUS, and then annually. They responded to International Consultation on Incontinence Questionnaire-Short Form (ICIQ-SF), International Prostate Symptom Score (IPSS), and Overactive Bladder Symptom Score (OABSS) questionnaires in every visit. Uroflowmetry and post-void residual volume (PVR) was examined at 0, 3, 24 months after the activation, and then biennially. According to the history of prior RT, the patients were divided into RT group (n = 20) and non-RT group (n= 56). We evaluated the longitudinal changes in ICIQ-SF, IPSS, OABSS, maximum flow rate (MFR), voided volume (VV), and PVR of the both groups using linear mixed model.
Results: The median age and follow-up duration of the whole cohort were 72 years and 40 months. Preoperative ICIQ-SF, IPSS, and OABSS in RT/non-RT groups were 17.6/18.0, 15.0/15.2, and 8.7/8.2, respectively. The corresponding scores at 1 month after activation were 4.5/5.0, 9.8/9.2, and 4.2/4.5, and all of them significantly improved. In the RT group, ICIQ-SF, IPSS, and OABSS subsequently deteriorated with a slope of 0.624 (P <0.01), 0.550 (P=0.02), and 0.298/year (P <0.01), respectively. In the non-RT group, no significant longitudinal changes in subsequent IPSS (0.156/year, P=0.57) and OABSS (-0.292/year, P=0.82) were observed although ICIQ-SF significantly deteriorated (0.431/year, P<0.01). Of MFR, VV, and PVR in the RT/non-RT group, VV in the RT group significantly deteriorated from 214 mL with a slope of -13.9 mL/year (P=0.02), while the other parameters did not show significant longitudinal changes.
Conclusions: Unlike in non-irradiated patients, improved LUTS after AUS implantation longitudinally deteriorated in patients undergoing RT. It could be result from the reduced bladder compliance due to the prior RT.
Source of Funding: None
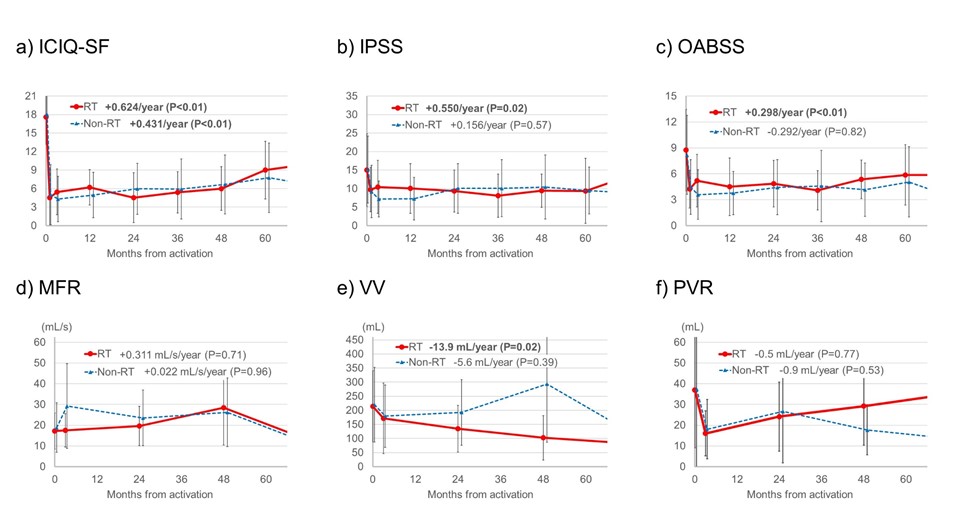
Methods: The current study included 76 patients receiving initial AUS implantation between 2010 and 2020. In principle, the patients were followed 1, 3, and 12 months after activation of the implanted AUS, and then annually. They responded to International Consultation on Incontinence Questionnaire-Short Form (ICIQ-SF), International Prostate Symptom Score (IPSS), and Overactive Bladder Symptom Score (OABSS) questionnaires in every visit. Uroflowmetry and post-void residual volume (PVR) was examined at 0, 3, 24 months after the activation, and then biennially. According to the history of prior RT, the patients were divided into RT group (n = 20) and non-RT group (n= 56). We evaluated the longitudinal changes in ICIQ-SF, IPSS, OABSS, maximum flow rate (MFR), voided volume (VV), and PVR of the both groups using linear mixed model.
Results: The median age and follow-up duration of the whole cohort were 72 years and 40 months. Preoperative ICIQ-SF, IPSS, and OABSS in RT/non-RT groups were 17.6/18.0, 15.0/15.2, and 8.7/8.2, respectively. The corresponding scores at 1 month after activation were 4.5/5.0, 9.8/9.2, and 4.2/4.5, and all of them significantly improved. In the RT group, ICIQ-SF, IPSS, and OABSS subsequently deteriorated with a slope of 0.624 (P <0.01), 0.550 (P=0.02), and 0.298/year (P <0.01), respectively. In the non-RT group, no significant longitudinal changes in subsequent IPSS (0.156/year, P=0.57) and OABSS (-0.292/year, P=0.82) were observed although ICIQ-SF significantly deteriorated (0.431/year, P<0.01). Of MFR, VV, and PVR in the RT/non-RT group, VV in the RT group significantly deteriorated from 214 mL with a slope of -13.9 mL/year (P=0.02), while the other parameters did not show significant longitudinal changes.
Conclusions: Unlike in non-irradiated patients, improved LUTS after AUS implantation longitudinally deteriorated in patients undergoing RT. It could be result from the reduced bladder compliance due to the prior RT.
Source of Funding: None

.jpg)
.jpg)