Back
Poster, Podium & Video Sessions
Moderated Poster
MP52: Urodynamics/Lower Urinary Tract Dysfunction/Female Pelvic Medicine: Male Incontinence: Therapy
MP52-10: Early Artificial Urinary Sphincter Placement and Device Survival After Bladder Neck Contracture Treatment: What is the Evidence?
Monday, May 16, 2022
7:00 AM – 8:15 AM
Location: Room 228
Samantha Nealon*, Raj Bhanvadia, Shervin Bhadkhshan, Sarah Sanders, Steve Hudak, Allen Morey, Dallas, TX
- SN
Poster Presenter(s)
Introduction: The impact of bladder neck stenosis on artificial urinary sphincter (AUS) outcomes is unknown. We present a comparative AUS survival analysis in patients with and without bladder neck contracture (BNC) treatment. We also sought to validate an institutional practice of 8-week post op cystoscopy to confirm bladder neck patency before AUS placement.
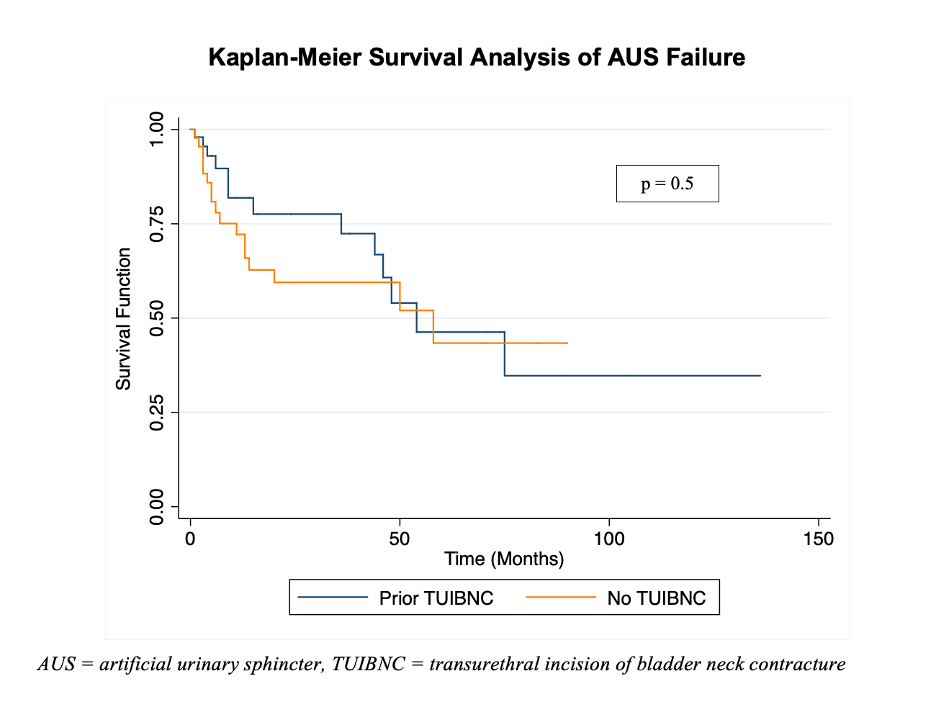
Methods: Retrospective review identified patients who underwent transurethral incision of bladder neck contracture (TUIBNC) followed by AUS placement for stress urinary incontinence (SUI) from 2008-2020. After a standardized endoscopic approach to the BNC, all patients had cystoscopy at 8 weeks to confirm bladder neck patency before AUS placement 1 month later. AUS survival in the BNC group was compared to a randomly selected group of AUS patients without BNC in the same period. Patient demographics and comorbidities were analyzed. A Cox Proportional Hazards model and Kaplan-Meier survival curve were generated comparing rates of AUS failure among BNC and non-BNC groups. Survival models were adjusted for age, BMI, and radiation history. Failure was defined as need for revision or explant.
Results: Of 893 AUS patients reviewed, 50 (5.6%) had a history of BNC and underwent preliminary TUIBNC. When bladder neck patency was confirmed at 8-week cystoscopy, AUS was scheduled. Recurrent BNC after AUS placement occurred in only 3/50 (6%) at median 2.5 months. All were managed successfully with repeat TUIBNC. On multivariable Cox analysis, prior TUIBNC was not associated with worse AUS survival. On Kaplan-Meier analysis, AUS survival was similar for BNC vs non-BNC groups, with 48-month survival of 61% and 59%, (p=0.5). Between BNC and non-BNC groups there was no difference in demographics, diabetes, radiation, need for revision (8/50, 16% vs 11/50, 22%), or cuff erosion (5/50, 10% vs. 6/50, 12%).
Conclusions: Over long-term follow up, AUS survival was similar to non-BNC controls. Cystoscopy at 8 weeks is a reliable indicator of long-term bladder neck patency, thus facilitating early AUS placement. For those with SUI after BNC treatment, early AUS placement is safe and effective.
Source of Funding: N/A
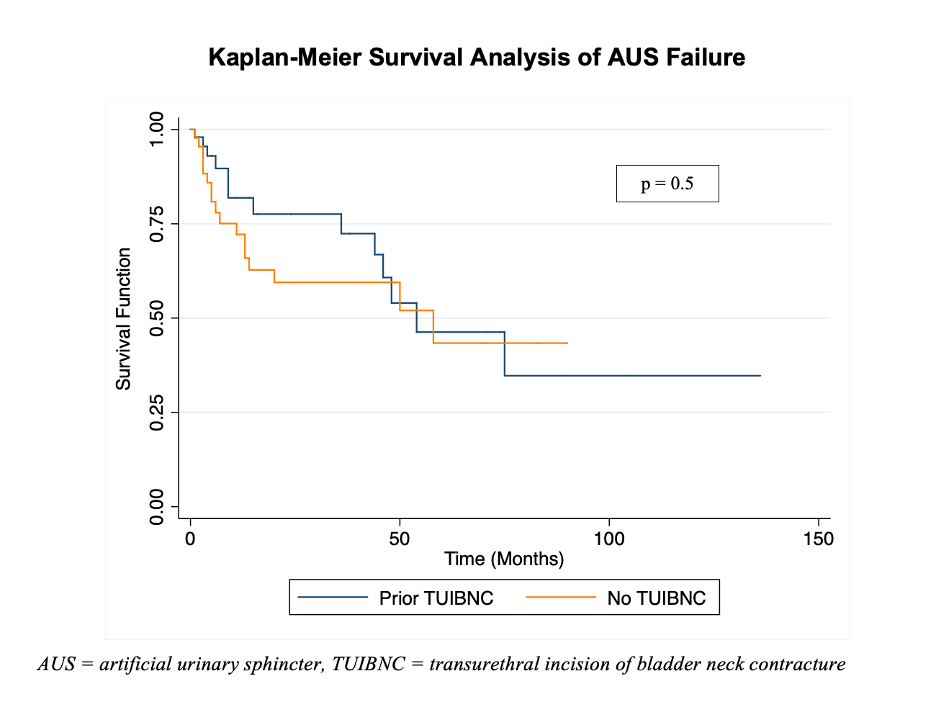
Methods: Retrospective review identified patients who underwent transurethral incision of bladder neck contracture (TUIBNC) followed by AUS placement for stress urinary incontinence (SUI) from 2008-2020. After a standardized endoscopic approach to the BNC, all patients had cystoscopy at 8 weeks to confirm bladder neck patency before AUS placement 1 month later. AUS survival in the BNC group was compared to a randomly selected group of AUS patients without BNC in the same period. Patient demographics and comorbidities were analyzed. A Cox Proportional Hazards model and Kaplan-Meier survival curve were generated comparing rates of AUS failure among BNC and non-BNC groups. Survival models were adjusted for age, BMI, and radiation history. Failure was defined as need for revision or explant.
Results: Of 893 AUS patients reviewed, 50 (5.6%) had a history of BNC and underwent preliminary TUIBNC. When bladder neck patency was confirmed at 8-week cystoscopy, AUS was scheduled. Recurrent BNC after AUS placement occurred in only 3/50 (6%) at median 2.5 months. All were managed successfully with repeat TUIBNC. On multivariable Cox analysis, prior TUIBNC was not associated with worse AUS survival. On Kaplan-Meier analysis, AUS survival was similar for BNC vs non-BNC groups, with 48-month survival of 61% and 59%, (p=0.5). Between BNC and non-BNC groups there was no difference in demographics, diabetes, radiation, need for revision (8/50, 16% vs 11/50, 22%), or cuff erosion (5/50, 10% vs. 6/50, 12%).
Conclusions: Over long-term follow up, AUS survival was similar to non-BNC controls. Cystoscopy at 8 weeks is a reliable indicator of long-term bladder neck patency, thus facilitating early AUS placement. For those with SUI after BNC treatment, early AUS placement is safe and effective.
Source of Funding: N/A

.jpg)
.jpg)