Back
Poster, Podium & Video Sessions
Moderated Poster
MP52: Urodynamics/Lower Urinary Tract Dysfunction/Female Pelvic Medicine: Male Incontinence: Therapy
MP52-19: Comparison of in-person FPMRS-directed pelvic floor therapy program versus unsupervised pelvic floor exercises following prostatectomy
Monday, May 16, 2022
7:00 AM – 8:15 AM
Location: Room 228
Jacques Farhi*, Anthony DeNovio, David Barquin, David Rapp, Charlottesville, VA

Jacques J. Farhi, MD, MBA
University of Virginia
Poster Presenter(s)
Introduction: Post-prostatectomy incontinence is common and associated with a high degree of patient distress. The UVA prostatectomy functional outcomes program (PFOP) was developed to comprehensively assess and optimize continence outcomes following robotic-assisted laparoscopic prostatectomy (RALP). Enrolled PFOP patients complete specialized in-person pelvic floor muscle training with a FPMRS specialist (DR), performed at baseline, 3-months, 6-months, and 12-months following surgery and supplemented by a home exercise program. This study compared continence outcomes in PFOP patients versus those receiving standard unsupervised home pelvic floor exercise therapy (UPFE) as directed by their urologic surgeon.
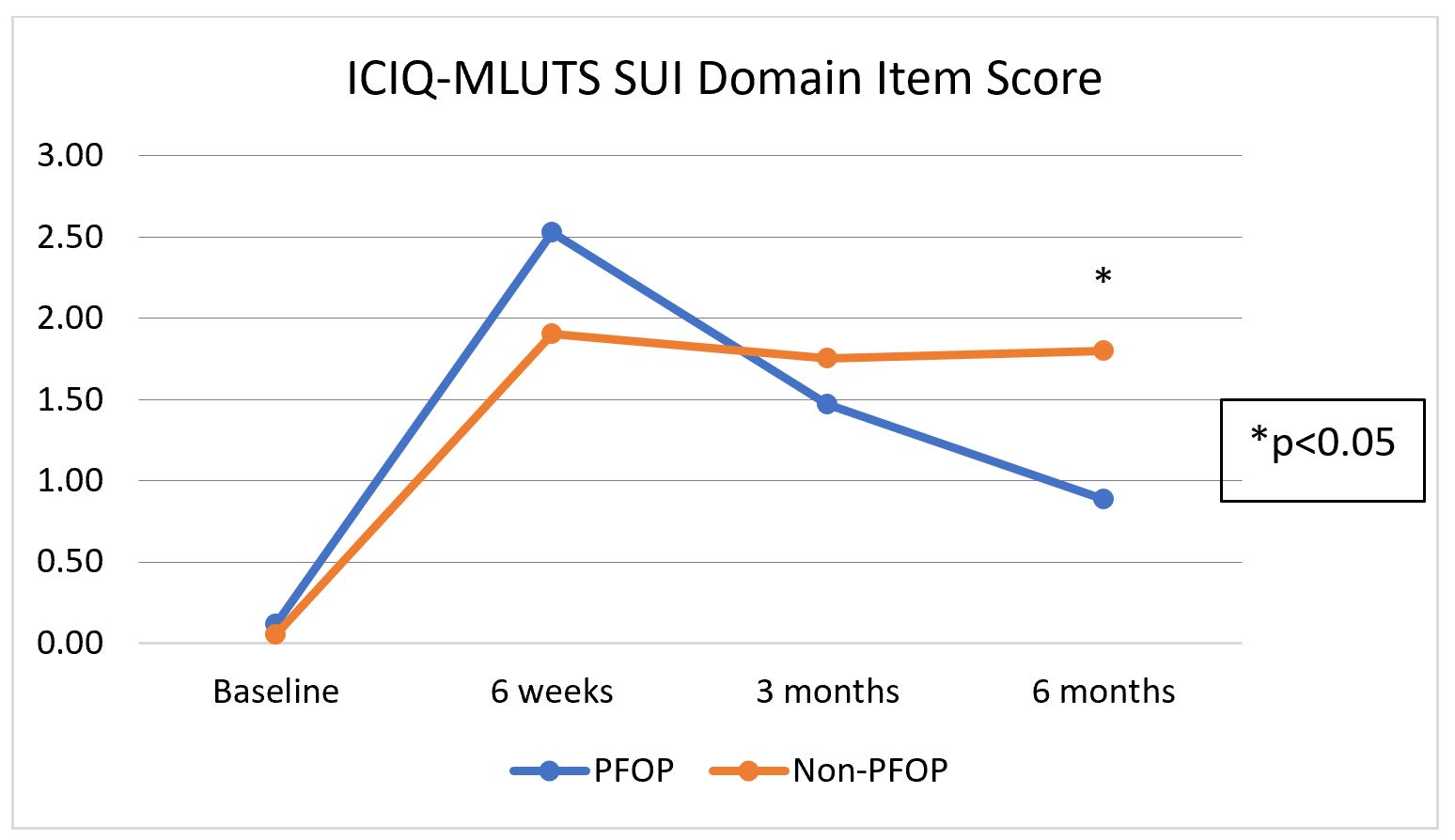
Methods: We performed a retrospective review of patients receiving PFMT versus UPFE with minimum 6-month follow-up. Incontinence and quality of life outcomes in all patients are prospectively assessed using the validated ICIQ-MLUTS and IIQ-7 questionnaires, in addition to items assessing daily pad use and satisfaction. Primary study outcomes included ICIQ-MLUTS SUI domain score and SUI cure (ICIQ SUI domain score = 0).
Results: Analysis included a total of 18 and 20 men with minimum 6-month follow-up receiving PFOP versus UPFE, respectively. No difference in patient age (62 vs 64 years), EBL (226 vs 182 ml), proportion of patients undergoing adjuvant radiotherapy (11% vs 10%), lymph node dissection (90% vs 85%), or baseline ICIQ SUI domain score (0.11 vs 0.05) was seen in comparison of PFOP versus UPFE cohorts (p=NS, all comparisons). Mean ICIQ-MLUTS SUI domain items scores across all time points are shown in Figure 1. At 6-month follow-up, men enrolled in PFOP demonstrated significantly improved SUI domain scores when compared to controls (PFOP 0.83 (SD 1.10); UPFE 1.8 (SD 1.47))(p < 0.05). Similarly, a higher proportion of PFOP patients reported SUI cure (PFOP 50%; UPFE 25%)(p=0.10). Similar pad per day quantity was reported across the cohorts (PFOP 0.89 (SD 1.02); UPFE 1.0 (SD 1.38))(p=NS).
Conclusions: In-person, FMPRS-directed PFMT is associated with improved SUI outcomes following RALP at 6-month follow-up. Further follow-up is ongoing to comprehensively assess outcomes through 1-year follow-up.
Source of Funding: None.
Methods: We performed a retrospective review of patients receiving PFMT versus UPFE with minimum 6-month follow-up. Incontinence and quality of life outcomes in all patients are prospectively assessed using the validated ICIQ-MLUTS and IIQ-7 questionnaires, in addition to items assessing daily pad use and satisfaction. Primary study outcomes included ICIQ-MLUTS SUI domain score and SUI cure (ICIQ SUI domain score = 0).
Results: Analysis included a total of 18 and 20 men with minimum 6-month follow-up receiving PFOP versus UPFE, respectively. No difference in patient age (62 vs 64 years), EBL (226 vs 182 ml), proportion of patients undergoing adjuvant radiotherapy (11% vs 10%), lymph node dissection (90% vs 85%), or baseline ICIQ SUI domain score (0.11 vs 0.05) was seen in comparison of PFOP versus UPFE cohorts (p=NS, all comparisons). Mean ICIQ-MLUTS SUI domain items scores across all time points are shown in Figure 1. At 6-month follow-up, men enrolled in PFOP demonstrated significantly improved SUI domain scores when compared to controls (PFOP 0.83 (SD 1.10); UPFE 1.8 (SD 1.47))(p < 0.05). Similarly, a higher proportion of PFOP patients reported SUI cure (PFOP 50%; UPFE 25%)(p=0.10). Similar pad per day quantity was reported across the cohorts (PFOP 0.89 (SD 1.02); UPFE 1.0 (SD 1.38))(p=NS).
Conclusions: In-person, FMPRS-directed PFMT is associated with improved SUI outcomes following RALP at 6-month follow-up. Further follow-up is ongoing to comprehensively assess outcomes through 1-year follow-up.
Source of Funding: None.

.jpg)
.jpg)