Back
Poster, Podium & Video Sessions
Moderated Poster
MP55: Prostate Cancer: Localized: Ablative Therapy
MP55-14: Salvage Robotic Radical Prostatectomy after Focal Therapy versus Radiation: a 10-Year Experience
Monday, May 16, 2022
8:45 AM – 10:00 AM
Location: Room 225
Alireza Ghoreifi*, Masatomo Kaneko, Hooman Djaladat, Andrew Hung, Rene Sotelo, Andre Berger, Mihir Desai, Inderbir Gill, Monish Aron, Andre Luis Abreu, Los Angeles, CA
Alireza Ghoreifi, MD
Research Fellow
University of Southern California
Poster Presenter(s)
Introduction: Salvage robotic radical prostatectomy (sRRP) has gained acceptance in the management of patients with recurrent prostate cancer. Limited data is available regarding the outcomes of this procedure, especially in the setting of primary focal therapy (FT). The aim of this study is to evaluate the outcomes of sRRP after primary FT versus radiation therapy (RT).
Methods: Using our IRB-approved prostate cancer database, we reviewed the records of patients who underwent sRRP following primary local therapy for prostate cancer between Jan 2010 to July 2021. Patients with concomitant procedures, including fistula repair and urethroplasty were excluded. Perioperative findings and long-term outcomes were recorded and compared between FT and RT groups.
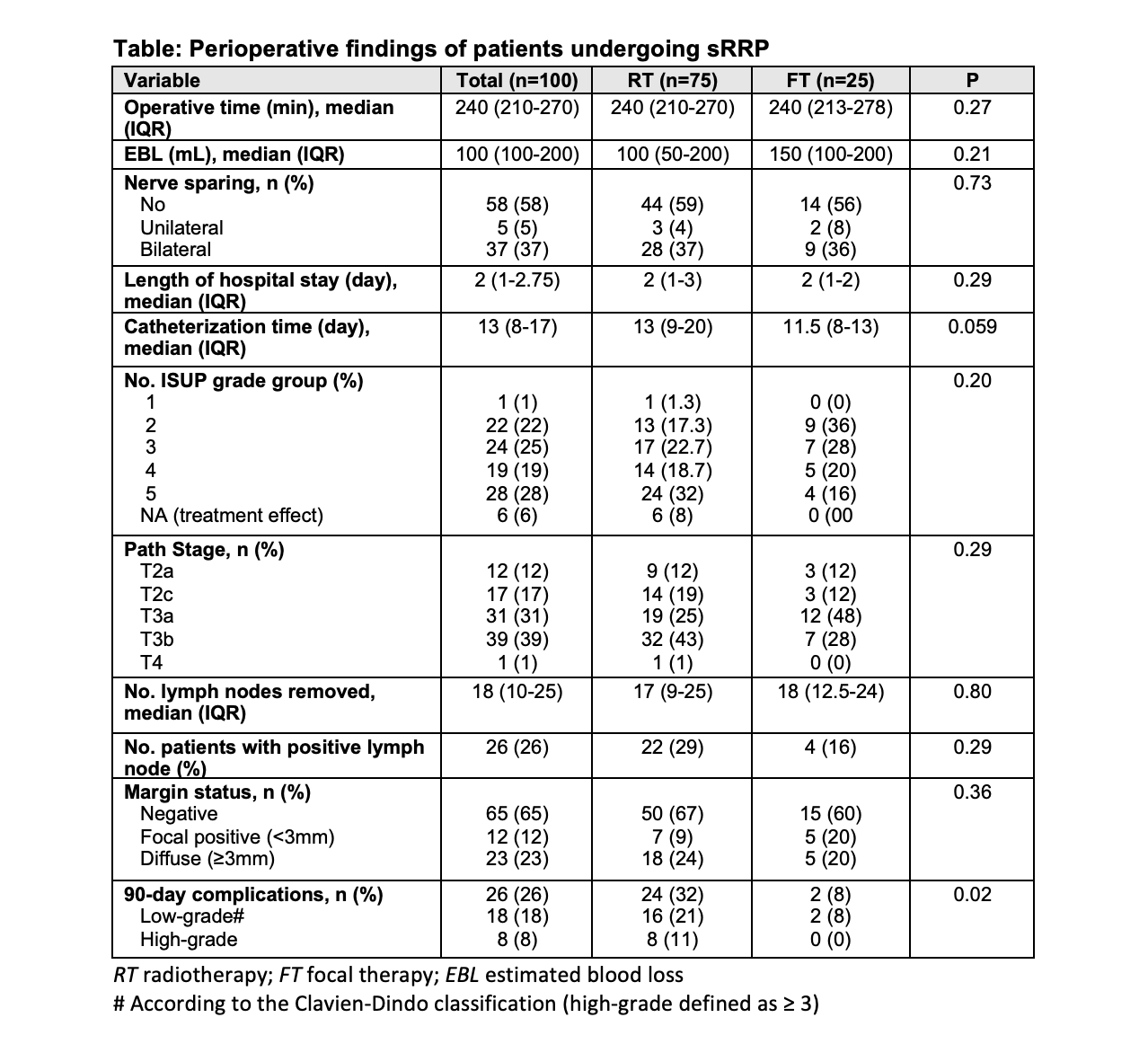
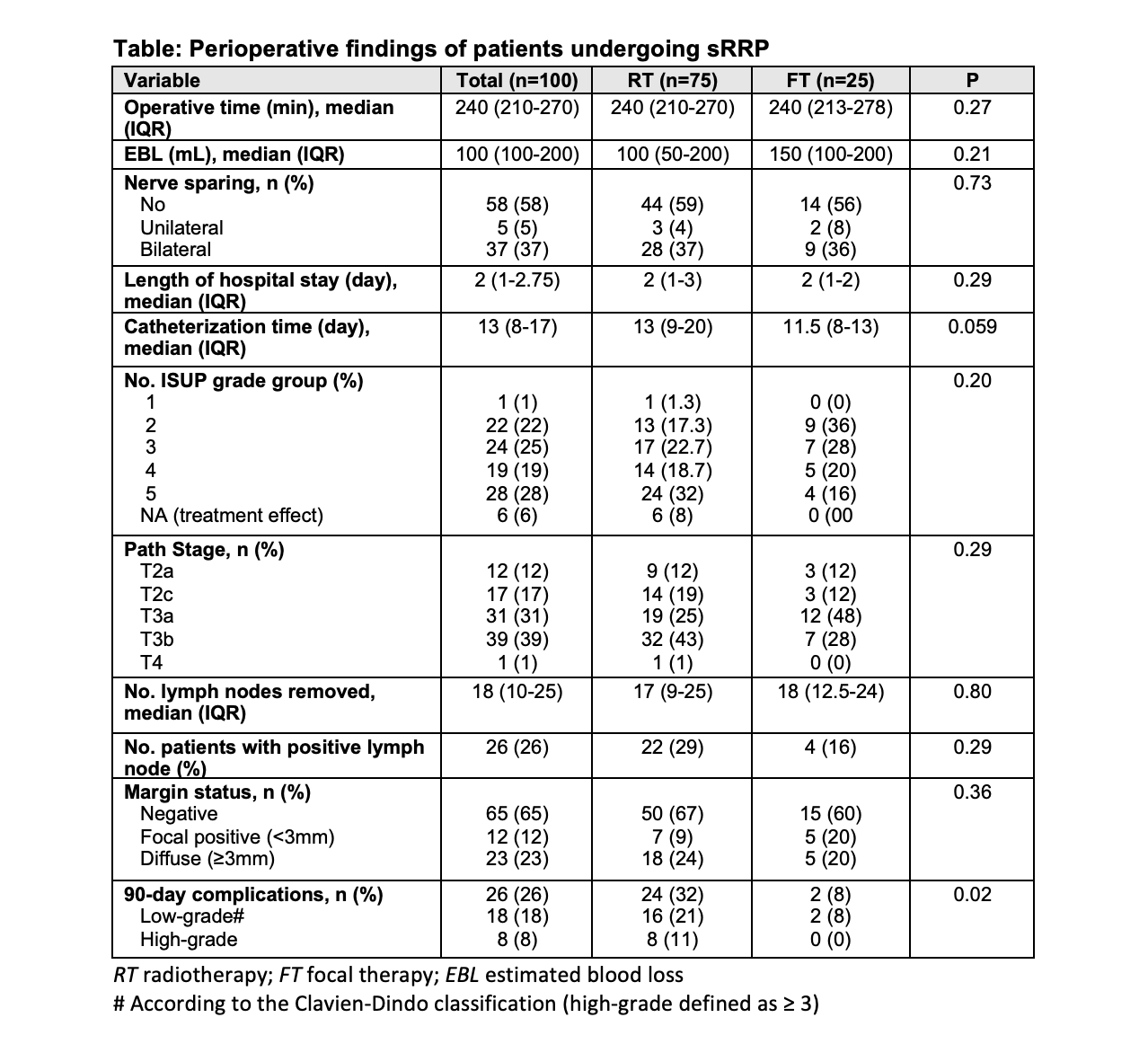
Results: A total of 100 patients with a median (IQR) age of 68 (63-74) years were included in the final analysis. Of these, 75 received RT (brachy=24, external beam=48, both=3) and 25 FT (Cryo=15, HIFU=8, both=1, focal laser ablation=1) as primary treatment. Median (IQR) time between primary treatment and sRRP was 66 (37-108) months (RT = 82 vs FT = 38M, p=0.0002). The median pre-sRRP PSA in RT vs. FT was 7.6 and 4.95 ng/mL, respectively (p=0.04). Pre-sRRP biopsy showed significantly higher rate of high-grade (GG = 4) cancer in RT compared to FT (33% vs. 20%, p=0.02). Perioperative and pathology findings are reported in the Table. There was 1 rectal injury in the RT group. 90-day complications were significantly higher in RT vs. FT patients (32% vs. 8%, p=0.02). 6-month, but not 12-month continence (defined as no pad usage) was higher in FT compared to RT (53% vs. 21%, p=0.02 and 67% vs. 35%, p=0.13). A total of 24 patients underwent artificial urethral sphincter (AUS) placement, all of whom were in the RT group. In a median (IQR) follow-up of 24 (5-52) months (RT = 24M vs. FT = 9M; p=0.30), 14 patients developed biochemical recurrence (PSA>0.2ng/mL), as follows: RT=15% vs. FT=12.5%. On multivariable analysis, history of RT was associated with higher rate of 90-day complications (Odds Ratio=4.9, 95% CI 1.06-23.02, p=0.04).
Conclusions: Salvage robotic radical prostatectomy in patients with recurrent prostate cancer following focal therapy is safe. It is associated with lower 90-day complications and earlier urinary continence compared to the patients who received primary radiotherapy.
Source of Funding: None
Methods: Using our IRB-approved prostate cancer database, we reviewed the records of patients who underwent sRRP following primary local therapy for prostate cancer between Jan 2010 to July 2021. Patients with concomitant procedures, including fistula repair and urethroplasty were excluded. Perioperative findings and long-term outcomes were recorded and compared between FT and RT groups.
Results: A total of 100 patients with a median (IQR) age of 68 (63-74) years were included in the final analysis. Of these, 75 received RT (brachy=24, external beam=48, both=3) and 25 FT (Cryo=15, HIFU=8, both=1, focal laser ablation=1) as primary treatment. Median (IQR) time between primary treatment and sRRP was 66 (37-108) months (RT = 82 vs FT = 38M, p=0.0002). The median pre-sRRP PSA in RT vs. FT was 7.6 and 4.95 ng/mL, respectively (p=0.04). Pre-sRRP biopsy showed significantly higher rate of high-grade (GG = 4) cancer in RT compared to FT (33% vs. 20%, p=0.02). Perioperative and pathology findings are reported in the Table. There was 1 rectal injury in the RT group. 90-day complications were significantly higher in RT vs. FT patients (32% vs. 8%, p=0.02). 6-month, but not 12-month continence (defined as no pad usage) was higher in FT compared to RT (53% vs. 21%, p=0.02 and 67% vs. 35%, p=0.13). A total of 24 patients underwent artificial urethral sphincter (AUS) placement, all of whom were in the RT group. In a median (IQR) follow-up of 24 (5-52) months (RT = 24M vs. FT = 9M; p=0.30), 14 patients developed biochemical recurrence (PSA>0.2ng/mL), as follows: RT=15% vs. FT=12.5%. On multivariable analysis, history of RT was associated with higher rate of 90-day complications (Odds Ratio=4.9, 95% CI 1.06-23.02, p=0.04).
Conclusions: Salvage robotic radical prostatectomy in patients with recurrent prostate cancer following focal therapy is safe. It is associated with lower 90-day complications and earlier urinary continence compared to the patients who received primary radiotherapy.
Source of Funding: None

.jpg)
.jpg)