Back
Poster, Podium & Video Sessions
Podium
PD05: Stone Disease: Medical & Dietary Therapy
PD05-09: Improved Stone Quality of Life in Patients with Obstructing Ureteral Stone on Alpha-Blocker Medical Expulsive Therapy
Friday, May 13, 2022
10:50 AM – 11:00 AM
Location: Room 252
Brijesh Patel*, St. Louis, MO, Tarik Phillips, Joshua Palk, Joel Vetter, St. Loius, MO, Mark Biebel, St. Louis, MO, Alexander Chow, Chicago, IL, Alethea Paradis, Alana Desai, St. Louis, MO, Kenneth Sands, Ramakrishna Venkatesh, St. Loius, MO
- BP
Podium Presenter(s)
Introduction: Though controversial, alpha blockers continue to be used widely for ureteral stone passage. However, its effects on the patient reported Quality of life (QOL), either positive, negative or no impact, is unknown. We compared the QoL of patients on alpha-blocker medical expulsive therapy (MET) to patients not on MET (noMET) utilizing a validated Wisconsin Stone Quality of Life (WISQOL).
Methods: After IRB approval, we performed a prospective study including patients on either MET or no MET after presenting to a tertiary-care ED with symptomatic, obstructing ureteral stones. Medical treatment type was decided at the point of care by the initial treating physician including medications for analgesia and nausea. Additionally, tamsulosin (0.4mg orally, daily) was prescribed for the MET group. The WISQOL survey was administered at baseline, 7-, 14-, 21- and 28-days following discharge from the ED or until stone expulsion.
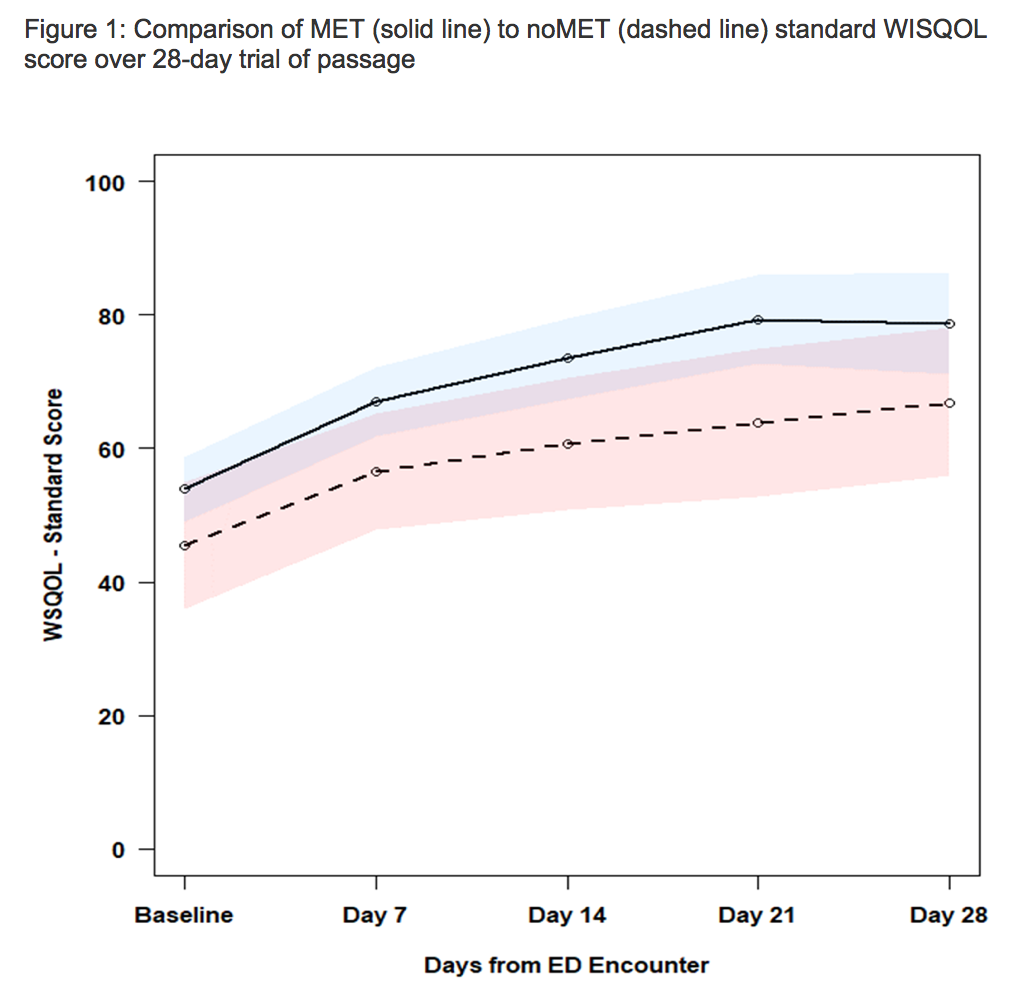
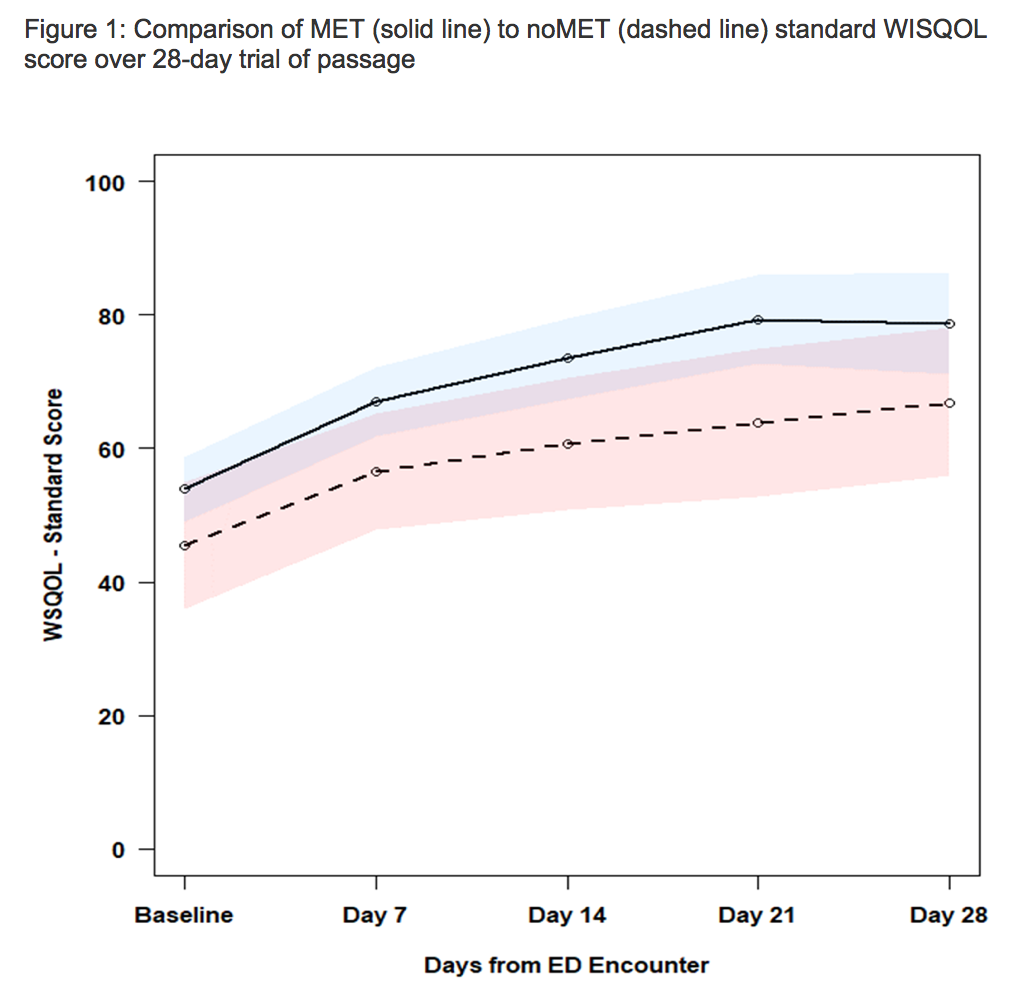
Results: A total of 197 patients were enrolled, of which 116 (59.2%) completed questionnaires for analysis, 91 in the MET group and 25 in no MET. Average ureteral stone size was 4.7 (STD 1.8) mm and 3.1 (STD 1.0) mm for MET and no MET, respectively. Of completed surveys, 105 (90%) were completed at day 7, 67 (57.6%) at day 14, 53 (45.7%) at day 21, and 40 (34.5%) at day 28. Spontaneous stone passage occurred in 38 (41.8%) while on MET compared to the 7 (28.0%) in no MET (p = 0.21). In total, 8 (6.8%) patients returned to the ED for intractable pain and 11 (9.5%) required surgical intervention. MET was associated with an improved QoL scores across all WISQOL domains compared to no MET (Fig.1). Stone size, age, race, sex, comorbidity score and a prior stone history were not associated with risk of negative effect on QoL (Table 1).
Conclusions: Use of alpha-blocker MET was associated with improved QOL on all WISQOL metrics compared to no MET patients. Larger, randomized controlled trial studies may validate these findings. Alpha-blocker treatment may be an indication to improve stone QOL in patients with ureteral stone colic.
Source of Funding: None

Methods: After IRB approval, we performed a prospective study including patients on either MET or no MET after presenting to a tertiary-care ED with symptomatic, obstructing ureteral stones. Medical treatment type was decided at the point of care by the initial treating physician including medications for analgesia and nausea. Additionally, tamsulosin (0.4mg orally, daily) was prescribed for the MET group. The WISQOL survey was administered at baseline, 7-, 14-, 21- and 28-days following discharge from the ED or until stone expulsion.
Results: A total of 197 patients were enrolled, of which 116 (59.2%) completed questionnaires for analysis, 91 in the MET group and 25 in no MET. Average ureteral stone size was 4.7 (STD 1.8) mm and 3.1 (STD 1.0) mm for MET and no MET, respectively. Of completed surveys, 105 (90%) were completed at day 7, 67 (57.6%) at day 14, 53 (45.7%) at day 21, and 40 (34.5%) at day 28. Spontaneous stone passage occurred in 38 (41.8%) while on MET compared to the 7 (28.0%) in no MET (p = 0.21). In total, 8 (6.8%) patients returned to the ED for intractable pain and 11 (9.5%) required surgical intervention. MET was associated with an improved QoL scores across all WISQOL domains compared to no MET (Fig.1). Stone size, age, race, sex, comorbidity score and a prior stone history were not associated with risk of negative effect on QoL (Table 1).
Conclusions: Use of alpha-blocker MET was associated with improved QOL on all WISQOL metrics compared to no MET patients. Larger, randomized controlled trial studies may validate these findings. Alpha-blocker treatment may be an indication to improve stone QOL in patients with ureteral stone colic.
Source of Funding: None


.jpg)
.jpg)