Back
Poster, Podium & Video Sessions
Podium
PD07: Prostate Cancer: Basic Research & Pathophysiology I
PD07-07: Molecular subtyping of >80,000 prostate cancer transcriptomes identifies four classes with distinct biological and clinical characteristics with implications for targeted therapies
Friday, May 13, 2022
10:30 AM – 10:40 AM
Location: Room 245
Adam Weiner*, Chicago, IL, Yang Liu, San Diego, CA, Ashley Ross, Chicago, IL, Felix Feng, San Francisco, CA, Phuoc Tran, Baltimore, MD, Nicholas Zaorsky, Hershey, PA, Angela Jia, Baltimore, MD, Xin Zhao, Alex Hakansson, Vinnie Liu, James Proudfoot, Ewan Gibb, Elai Davicioni, San Diego, CA, Daniel Spratt, Cleveland, OH, Edward Schaeffer, Chicago, IL
Podium Presenter(s)
Introduction: We used molecular subtyping to characterize the largest prostate cancer transcriptome database to understand the tumor behavior and help guide treatment decision making.
Methods: Whole transcriptome analyses was performed on de-identified tumor samples from biopsies or radical prostatectomy from the clinical use of the Decipher prostate genomic classifier (Decipher Biosciences, San Diego, CA; n=32,000, training cohort, n=48,703, testing cohort). We grouped these patients based on expression patterns of a curated panel of signatures and biomarkers relevant to systemic therapies for prostate cancer (n=21), from which we identified 4 clusters with distinct biological characteristics. A multinomial logistic regression was trained to reproduce the clusters as a single sample classifier.
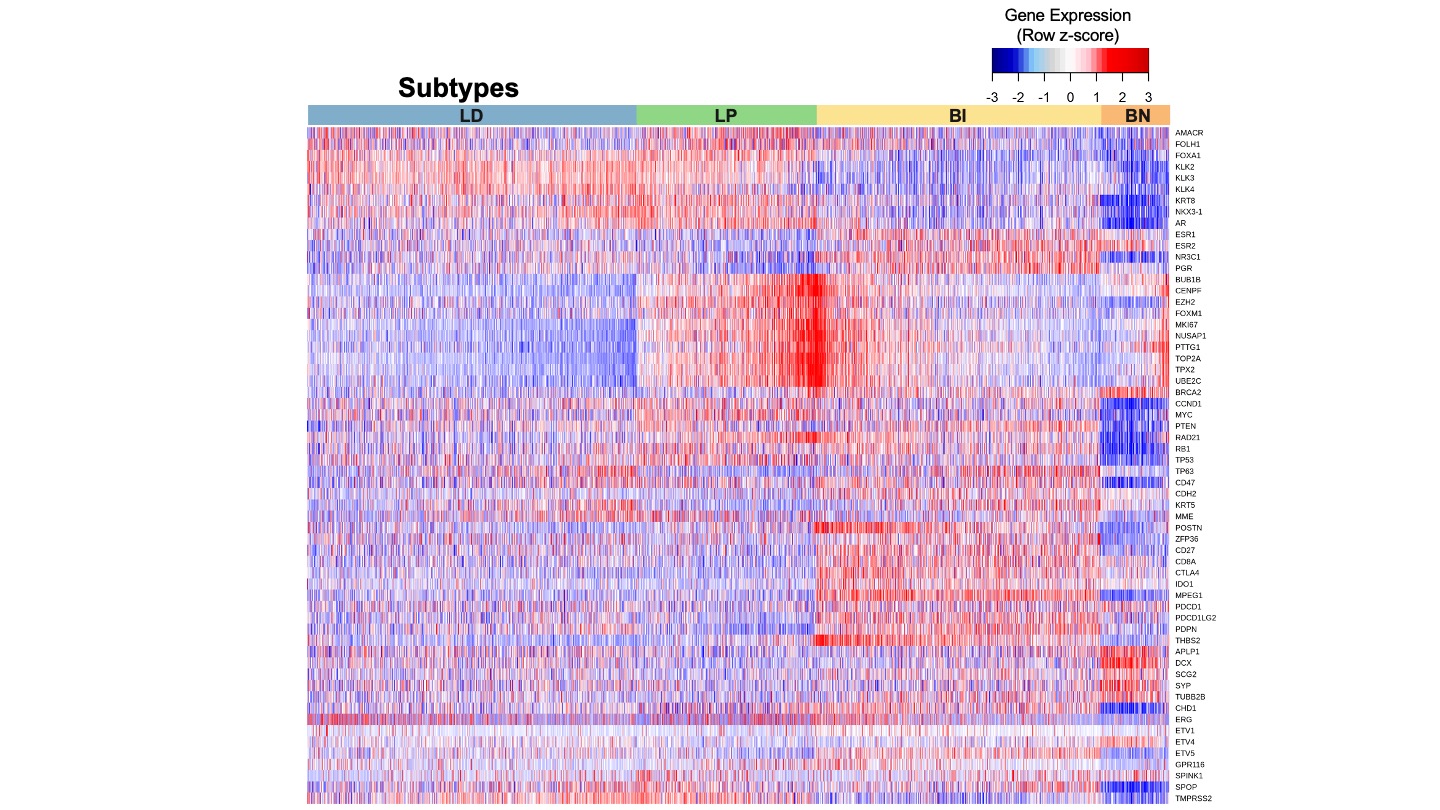
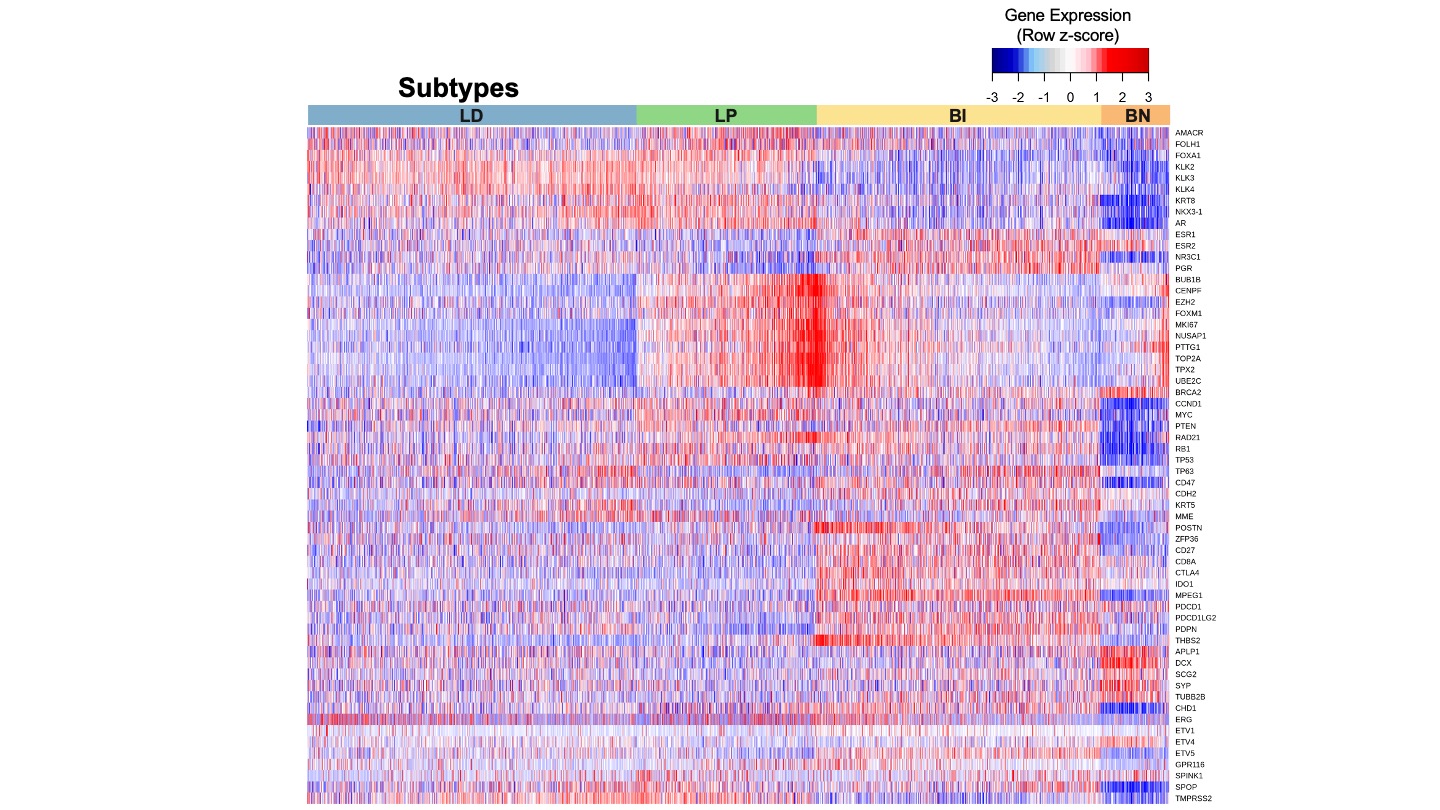
Results: Luminal-Differentiating (LD) tumors had the highest AR-activity scores, upregulation of canonical AR transcriptional targets (i.e., PSA and PSMA; Fig). Luminal Proliferating (LP) tumors had the highest expression of AR, and cell proliferation genes (e.g., MKI67 and TOP2A) and pathways. Basal Immune (BI) tumors possessed significant immune infiltration and T-effector cell activity and low levels of immune suppressor signatures. Basal Neuroendocrine (BN) tumors were characterized by low AR-activity expression, low immune infiltration, and enrichment with neuronal gene expression. LP and BI tumors tended to possess more aggressive clinical characteristics: high proportions of grade group 4-5, node positive disease (BI only), and high Decipher score. In a cohort of patients treated with radical prostatectomy (n=855), patients with LD tumors experienced longer metastasis-free survival compared to LP (HR=3.56 [1.83-6.93]), BI (HR=2.55 [1.29-5.01]) and BN (HR=3.30 [1.03-10.61]) with Cox regression adjusting for age, PSA, stage and Gleason score.
Conclusions: This molecular subtyping model for prostate cancer, derived from the largest reported transcriptome analysis of primary tumors segments tumors by relevant biological processes with potential implications for targeting systemic therapies.
Source of Funding: Decipher Biosciences
Methods: Whole transcriptome analyses was performed on de-identified tumor samples from biopsies or radical prostatectomy from the clinical use of the Decipher prostate genomic classifier (Decipher Biosciences, San Diego, CA; n=32,000, training cohort, n=48,703, testing cohort). We grouped these patients based on expression patterns of a curated panel of signatures and biomarkers relevant to systemic therapies for prostate cancer (n=21), from which we identified 4 clusters with distinct biological characteristics. A multinomial logistic regression was trained to reproduce the clusters as a single sample classifier.
Results: Luminal-Differentiating (LD) tumors had the highest AR-activity scores, upregulation of canonical AR transcriptional targets (i.e., PSA and PSMA; Fig). Luminal Proliferating (LP) tumors had the highest expression of AR, and cell proliferation genes (e.g., MKI67 and TOP2A) and pathways. Basal Immune (BI) tumors possessed significant immune infiltration and T-effector cell activity and low levels of immune suppressor signatures. Basal Neuroendocrine (BN) tumors were characterized by low AR-activity expression, low immune infiltration, and enrichment with neuronal gene expression. LP and BI tumors tended to possess more aggressive clinical characteristics: high proportions of grade group 4-5, node positive disease (BI only), and high Decipher score. In a cohort of patients treated with radical prostatectomy (n=855), patients with LD tumors experienced longer metastasis-free survival compared to LP (HR=3.56 [1.83-6.93]), BI (HR=2.55 [1.29-5.01]) and BN (HR=3.30 [1.03-10.61]) with Cox regression adjusting for age, PSA, stage and Gleason score.
Conclusions: This molecular subtyping model for prostate cancer, derived from the largest reported transcriptome analysis of primary tumors segments tumors by relevant biological processes with potential implications for targeting systemic therapies.
Source of Funding: Decipher Biosciences

.jpg)
.jpg)
