Back
Poster, Podium & Video Sessions
Bladder Cancer: Epidemiology & Evaluation I
PD14-01: Retrospective review of patients presenting to the emergency department with gross hematuria and newly diagnosed genitourinary malignancy: not as common as we thought?
Friday, May 13, 2022
3:30 PM – 3:40 PM
Location: Room 255
Deepansh Dalela*, Stephen Wertheimer, Jackson Darling, Callie Bartkowiak, Humphrey Atiemo, Detroit, MI

Deepansh Dalela, MD
Fellow
Vattikuti Urology Institute/Department of Urology, Henry Ford Hospital
Podium Presenter(s)
Introduction: Gross Hematuria (GH) is associated with up to 20-25% incidence of genitourinary (GU) malignancy. Given that the emergency department (ED) is often the first point of care for patients presenting with GH, we assessed the demographics of GH patients presenting to the ED and subsequently diagnosed with new genitourinary (GU) malignancy within a safety net, tertiary care health system over a one-year period.
Methods: Patients presenting with GH to six EDs within the Henry Ford Health System (Southeast Michigan) between 1/1/2019 to 12/31/2019 and subsequently newly diagnosed GU malignancy were evaluated with respect to relevant socio-demographic and tumor variables.
Results: Of the 286,313 ED presentations in 2019, 1370 had a diagnosis of GH (0.48%), and 19 (1.4%) were subsequently diagnosed with of GU cancer.
Median (IQR) age at diagnosis was 73 (68.5-84) years, 16% were Black, 26% female, 25% had family history of GU cancer and 58% were active smokers (average 42 pack year). Median household income was $54,168, 9% less than median state income. All patients were insured.
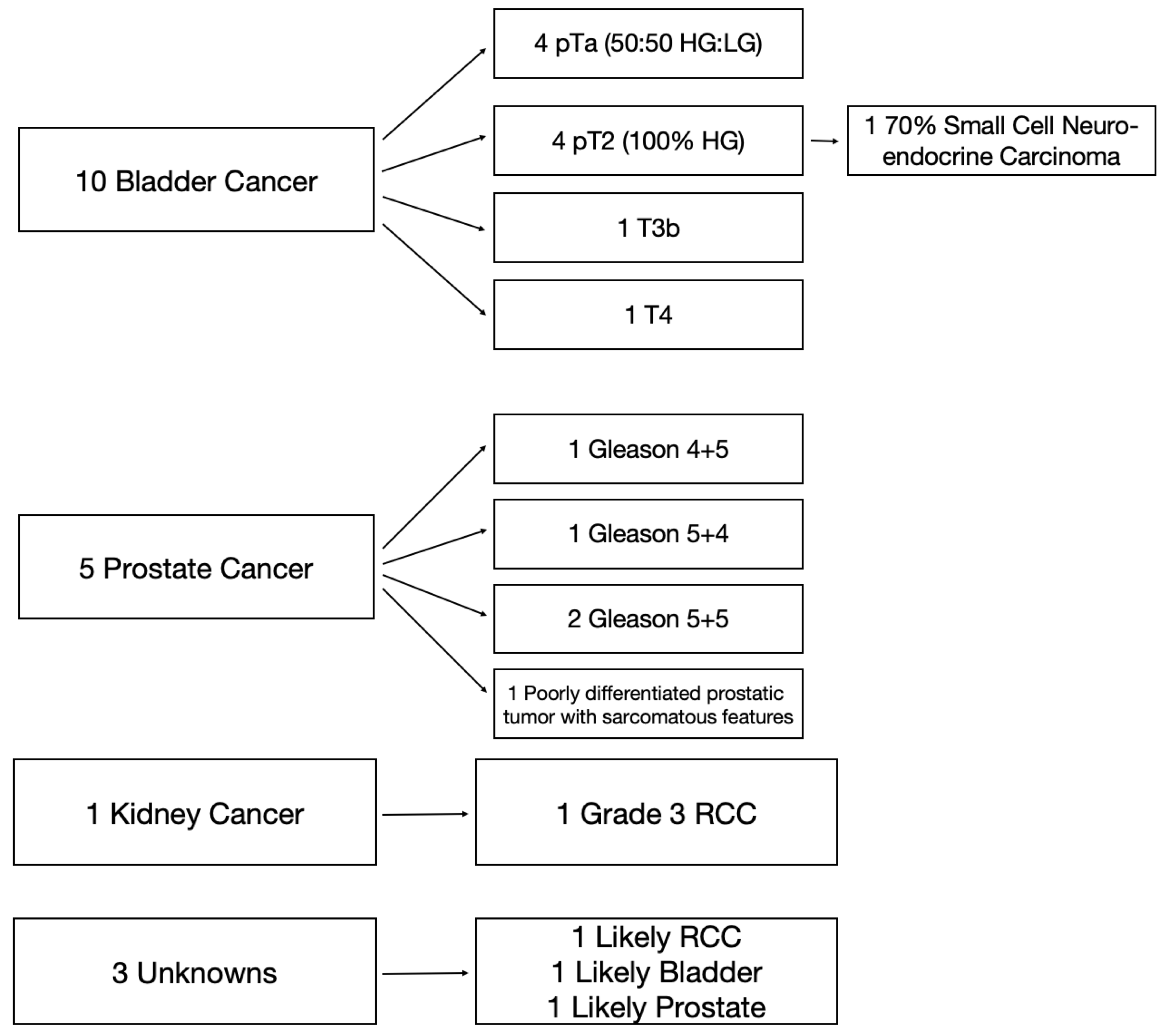
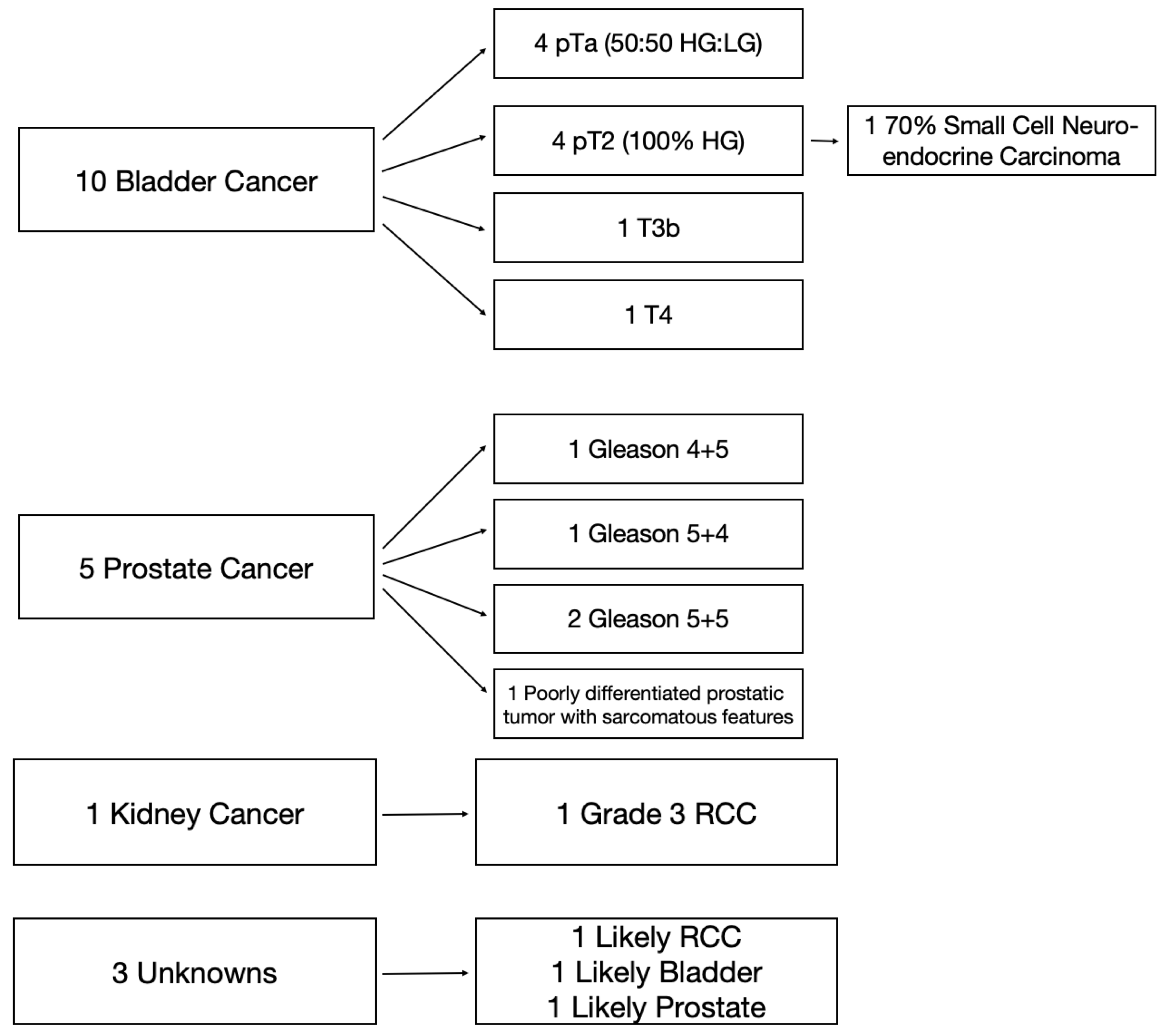
Median time to diagnosis was 33 days, which was reduced to 20 days if Urology was consulted. Bladder (53%) and prostate (26%) comprised the majority of newly diagnosed GU cancers (Figure 1)
Conclusions: Somewhat contrary to our hypothesis, GH represented ~0.5% of all ED visits, with a small proportion (1.4%) being diagnosed with new GU cancer. This may be related to stage migration (earlier detection of cancers with imaging), better insurance (100% of our cohort was insured) or better access to care (HFHS is a tertiary care, safety net hospital). While timely urology evaluation decreased time for diagnosis (33 to 20 days) and majority (53%) were newly diagnosed with bladder cancer, nearly half harbored advanced prostate or kidney cancer when presenting with GH. Limitations of our study include a short analytic cohort (1 year), lack of survival outcomes and single center data.
Source of Funding: n/a
Methods: Patients presenting with GH to six EDs within the Henry Ford Health System (Southeast Michigan) between 1/1/2019 to 12/31/2019 and subsequently newly diagnosed GU malignancy were evaluated with respect to relevant socio-demographic and tumor variables.
Results: Of the 286,313 ED presentations in 2019, 1370 had a diagnosis of GH (0.48%), and 19 (1.4%) were subsequently diagnosed with of GU cancer.
Median (IQR) age at diagnosis was 73 (68.5-84) years, 16% were Black, 26% female, 25% had family history of GU cancer and 58% were active smokers (average 42 pack year). Median household income was $54,168, 9% less than median state income. All patients were insured.
Median time to diagnosis was 33 days, which was reduced to 20 days if Urology was consulted. Bladder (53%) and prostate (26%) comprised the majority of newly diagnosed GU cancers (Figure 1)
Conclusions: Somewhat contrary to our hypothesis, GH represented ~0.5% of all ED visits, with a small proportion (1.4%) being diagnosed with new GU cancer. This may be related to stage migration (earlier detection of cancers with imaging), better insurance (100% of our cohort was insured) or better access to care (HFHS is a tertiary care, safety net hospital). While timely urology evaluation decreased time for diagnosis (33 to 20 days) and majority (53%) were newly diagnosed with bladder cancer, nearly half harbored advanced prostate or kidney cancer when presenting with GH. Limitations of our study include a short analytic cohort (1 year), lack of survival outcomes and single center data.
Source of Funding: n/a

.jpg)
.jpg)