Back
Poster, Podium & Video Sessions
Bladder Cancer: Epidemiology & Evaluation I
PD14-02: Critical Evaluation of the 2020 Microhematuria Guidelines: Are We Still Working Up Too Many Patients?
Friday, May 13, 2022
3:40 PM – 3:50 PM
Location: Room 255
Eric Macdonald*, Jacob Gaines, Max Kuster, Michelle Ou, Ella Taubenfeld, Adam Diamond, Tavya Benjamin, Michael Diefenbach, Manish Vira, Simon Hall, Lake Success, NY

Eric J. Macdonald
The Smith Institute for Urology
Podium Presenter(s)
Introduction: In 2020, the updated AUA/SUFU microhematuria (MH) guidelines were released. Due to limited supporting evidence, research is needed for validation and evaluation. We applied the guidelines to 1,906 patients with MH to determine percentage of positive workups in the current risk groups and analyze the clinical characteristics used for stratification.
Methods: We reviewed the records of all patients with MH (=3 RBCs/HPF) evaluated between 2010-2019. Patients with a history of gross hematuria were excluded. Only patients who received cystoscopy and imaging within 1 year of MH diagnosis were included. Patients were labeled low-risk (LoR), intermediate-risk (InR), or high-risk (HiR) per the new guidelines. Positive findings were divided into 3 groups for subgroup analysis: total neoplasms, urothelial cancer, and renal neoplasms.
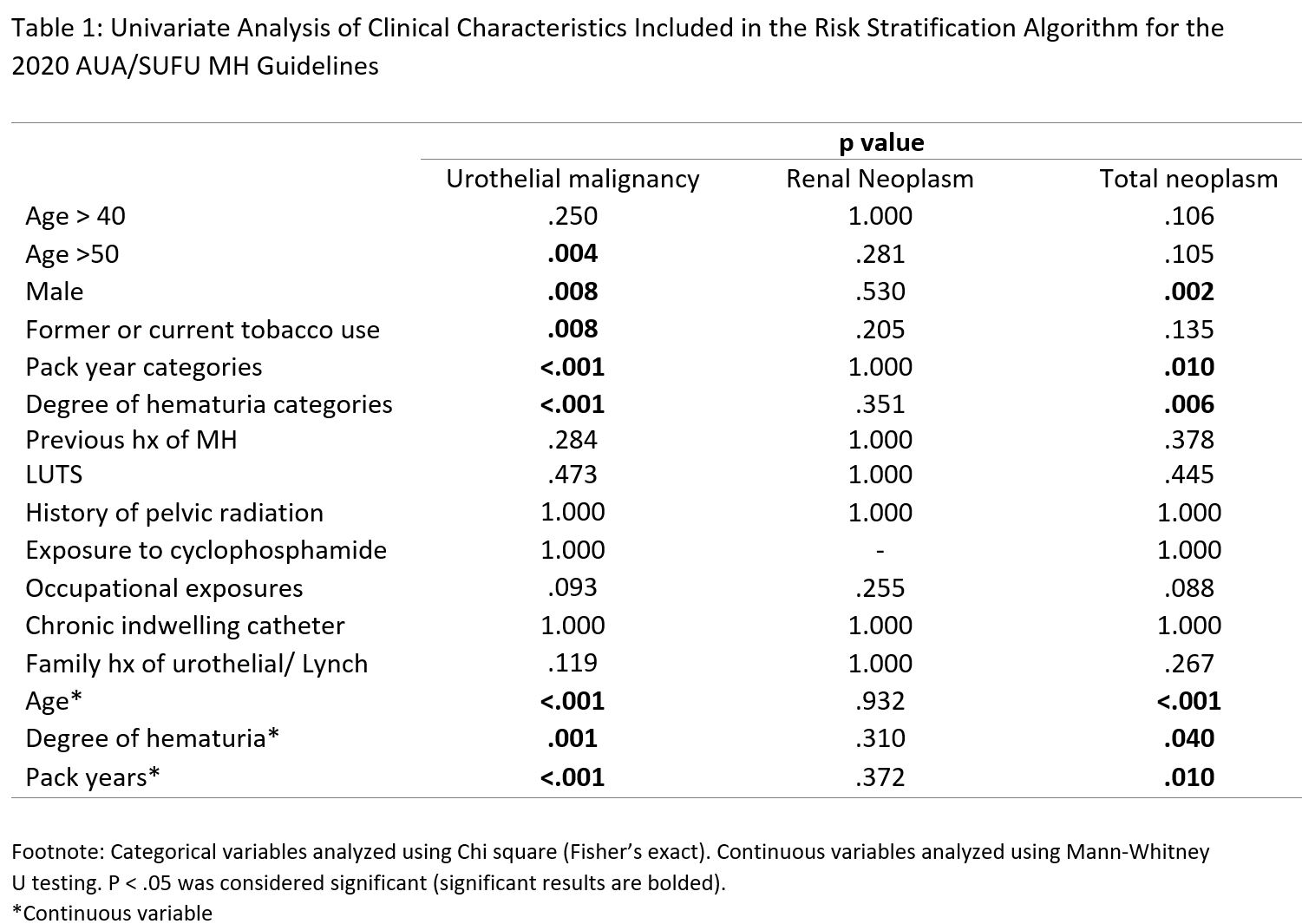
Results: Our cohort was divided into 3 risk groups: LoR (n=163, 8.55%), InR (n=733, 38.4%), and HiR (n=1,010, 53.0%). We identified 33 neoplasms (1.73% positivity) including 21 urothelial cancers and 12 renal neoplasms (4 pathologically confirmed and 8 suspicious by imaging). No LoR patients had a neoplasm. Within InR patients, 5 neoplasms were identified (0.68% positivity): 1 urothelial and 4 renal. Among HiR patients, 28 neoplasms were identified (2.77% positivity): 20 urothelial and 8 renal. Urothelial cancers included non-muscle invasive bladder cancers (n=19) and upper tract urothelial cancers (n=2), all stage T1 or below. Univariate analysis was performed on clinical factors included in the guidelines and reported in Table 1. Multivariate logistic regressions showed that only male sex and increasing age remained significant for total neoplasms (p <.05), but subgroup analysis demonstrated that former/current tobacco use also correlated with urothelial malignancy. No clinical factors were significantly associated with renal neoplasms.
Conclusions: The exceedingly low rates of malignancy discovered in our cohort suggest that the new MH guidelines can be further improved to reduce the burden of testing. Specifically, the 0.68% positivity rate in the InR group shows that workup could potentially be deferred for these patients. The lack of association for any clinical risk factor with renal neoplasms suggests that their discovery in this scenario may be coincidental.
Source of Funding: none
Methods: We reviewed the records of all patients with MH (=3 RBCs/HPF) evaluated between 2010-2019. Patients with a history of gross hematuria were excluded. Only patients who received cystoscopy and imaging within 1 year of MH diagnosis were included. Patients were labeled low-risk (LoR), intermediate-risk (InR), or high-risk (HiR) per the new guidelines. Positive findings were divided into 3 groups for subgroup analysis: total neoplasms, urothelial cancer, and renal neoplasms.
Results: Our cohort was divided into 3 risk groups: LoR (n=163, 8.55%), InR (n=733, 38.4%), and HiR (n=1,010, 53.0%). We identified 33 neoplasms (1.73% positivity) including 21 urothelial cancers and 12 renal neoplasms (4 pathologically confirmed and 8 suspicious by imaging). No LoR patients had a neoplasm. Within InR patients, 5 neoplasms were identified (0.68% positivity): 1 urothelial and 4 renal. Among HiR patients, 28 neoplasms were identified (2.77% positivity): 20 urothelial and 8 renal. Urothelial cancers included non-muscle invasive bladder cancers (n=19) and upper tract urothelial cancers (n=2), all stage T1 or below. Univariate analysis was performed on clinical factors included in the guidelines and reported in Table 1. Multivariate logistic regressions showed that only male sex and increasing age remained significant for total neoplasms (p <.05), but subgroup analysis demonstrated that former/current tobacco use also correlated with urothelial malignancy. No clinical factors were significantly associated with renal neoplasms.
Conclusions: The exceedingly low rates of malignancy discovered in our cohort suggest that the new MH guidelines can be further improved to reduce the burden of testing. Specifically, the 0.68% positivity rate in the InR group shows that workup could potentially be deferred for these patients. The lack of association for any clinical risk factor with renal neoplasms suggests that their discovery in this scenario may be coincidental.
Source of Funding: none

.jpg)
.jpg)