Back
Poster, Podium & Video Sessions
Podium
PD17: Prostate Cancer: Detection & Screening III
PD17-04: Prostate cancers detected at multi-parametric MRI targeted versus systematic biopsies: are they equal? Results from a large multi-institutional series.
Saturday, May 14, 2022
7:30 AM – 7:40 AM
Location: Room 252
Francesco Barletta*, Milano, Italy, Elio Mazzone, Giorgio Gandaglia, Milan, Italy, Guillaume Ploussard, Razvan-George Rahota, Toulouse, France, Massimo Valerio, Lausanne, Switzerland, Riccardo Campi, Andrea Mari, Florence, Italy, Agostino Mattei, Lucerne, Switzerland, Giancarlo Marra, Turin, Italy, Jean Baptiste Beauval, Mathieu Roumiguiè, Toulouse, France, Luca Afferi, Lucerne, Italy, Marco Moschini, Lucerne, Switzerland, Paolo Gontero, Turin, Italy, Roderick van den Bergh, Utrecht, Netherlands, Junlong Zhuang, Hongqian Tuo, Jiangsu, China, People's Republic of, Armando Stabile, Milan, Italy, Nicola Fossati, Lugano, Switzerland, Francesco De Cobelli, Antonio Esposito, Giorgio Brembilla, Francesco Montorsi, Alberto Briganti, Milan, Italy
- FB
Podium Presenter(s)
Introduction: Multiparametric magnetic resonance imaging of the prostate (mpMRI) and targeted biopsies (TBx) allows for improved detection of clinically significant prostate cancer (csPCa). However, whether PCa detected at mpMRI-TBx carry the same prognostic role as compared to tumors detected at concomitant systematic biopsies (SBx) is unknown. We aimed at comparing the impact of csPCa at TBx vs. SBx on pathologic and oncological outcomes after radical prostatectomy (RP).
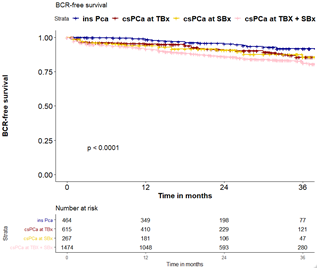
Methods: Overall, 3,434 PCa patients treated with RP at 9 centres between 2015 and 2020 were identified. All men received mpMRI for diagnostic purposes with a TBx plus SBx. The study outcomes were adverse pathology and biochemical recurrence (BCR, two PSA =0.2 ng/ml after RP) after RP. Multivariable logistic regression analyses (MVA) assessed the exclusive presence of csPCa at TBx or at SBx as a predictor of positive margins (PSM), extracapsular extension (ECE), and lymph-node invasion (LNI). Multivariable Cox regression analysis assessed predictors of BCR adjusting for PSA, grade at SBx, grade at TBx, pT stage and LNI. Adjusted Kaplan Meier analyses were used.
Results: Median age and PSA were 66 yrs and 7.3 ng/mL. Overall, 64% and 76% of men had csPCa at SBx and TBx. At RP, 48%, 22%, and 8% had pT3, PSM, and LNI. At MVA, the exclusive presence of csPCa at TBx was a predictor of ECE (OR: 1.98; all p<0.001) and LNI (OR: 10; p<0.001). The exclusive presence of csPCa at either TBx or at SBx, was associated with BCR (p=0.04). The exclusive presence of csPCa at TBx vs SBx similarly affected BCR-free survival (HR: 1.10 vs 1.08). The presence of csPCa at both SBx and TBx was associated with higher BCR rates (p=0.01).
Conclusions: csPCa detected at either TBx vs SBx had similar impact on BCR rate. Furthermore, the presence of csPCa at both SBx and TBx had the highest impact on BCR. A similar biological behaviour between csPCa detected at SBx vs TBx might be expected, underlining the importance of performing both TBx plus SBx in men with suspicious lesions at mpMRI.
Source of Funding: None.
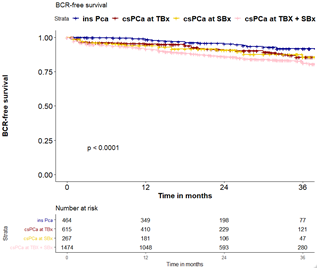
Methods: Overall, 3,434 PCa patients treated with RP at 9 centres between 2015 and 2020 were identified. All men received mpMRI for diagnostic purposes with a TBx plus SBx. The study outcomes were adverse pathology and biochemical recurrence (BCR, two PSA =0.2 ng/ml after RP) after RP. Multivariable logistic regression analyses (MVA) assessed the exclusive presence of csPCa at TBx or at SBx as a predictor of positive margins (PSM), extracapsular extension (ECE), and lymph-node invasion (LNI). Multivariable Cox regression analysis assessed predictors of BCR adjusting for PSA, grade at SBx, grade at TBx, pT stage and LNI. Adjusted Kaplan Meier analyses were used.
Results: Median age and PSA were 66 yrs and 7.3 ng/mL. Overall, 64% and 76% of men had csPCa at SBx and TBx. At RP, 48%, 22%, and 8% had pT3, PSM, and LNI. At MVA, the exclusive presence of csPCa at TBx was a predictor of ECE (OR: 1.98; all p<0.001) and LNI (OR: 10; p<0.001). The exclusive presence of csPCa at either TBx or at SBx, was associated with BCR (p=0.04). The exclusive presence of csPCa at TBx vs SBx similarly affected BCR-free survival (HR: 1.10 vs 1.08). The presence of csPCa at both SBx and TBx was associated with higher BCR rates (p=0.01).
Conclusions: csPCa detected at either TBx vs SBx had similar impact on BCR rate. Furthermore, the presence of csPCa at both SBx and TBx had the highest impact on BCR. A similar biological behaviour between csPCa detected at SBx vs TBx might be expected, underlining the importance of performing both TBx plus SBx in men with suspicious lesions at mpMRI.
Source of Funding: None.

.jpg)
.jpg)