Back
Poster, Podium & Video Sessions
Podium
PD19: Stone Disease: Surgical Therapy (including ESWL) II
PD19-07: Are patients stented for septic ureteral stones more likely to experience infectious complications at time of definitive management than those stented for non-infectious indications?
Saturday, May 14, 2022
8:00 AM – 8:10 AM
Location: Room 245
Ginnie Jeng*, Hempstead, NY, Simon J Hall, New Hyde Park, NY
- GJ
Podium Presenter(s)
Introduction: Current practices for septic ureteral stones include urgent decompression of the collecting system and antibiotic administration. Surgical management of the stone is delayed until infection has resolved. Therefore, the purpose of this study is to evaluate the rate of urosepsis after stenting, identify risk factors for developing urosepsis, and define optimal antibiotic prophylaxis for ureteroscopy (URS).
Methods: We conducted a retrospective cohort study of patients who underwent urgent ureteral stenting followed by URS with laser lithotripsy for urolithiasis management from January 2018 to December 2019 at Northwell Health. Data collected include patient demographics, stent indications, stone characteristics, blood and urine culture results, and antibiotics used. Statistical analyses include Pearson’s Chi Square analysis and Fisher’s Exact test, with p values <0.05 considered statistically significant.
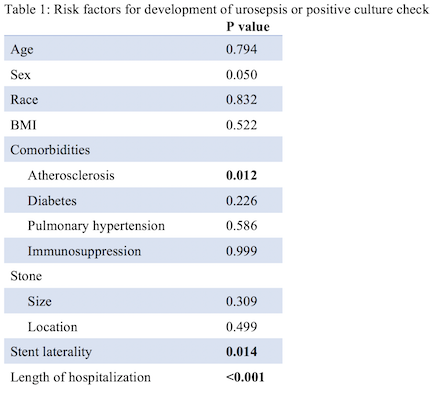
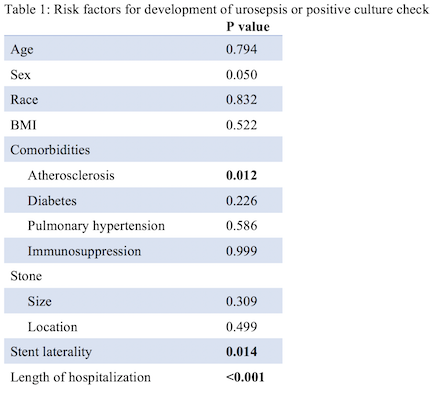
Results: 181 patients were included in this study, with 88 stented for urosepsis concerns (Sepsis Group, SG) and 92 for intractable pain or acute kidney injury (Non-Sepsis Group, NSG). SG is significantly more likely to have a positive culture check (SG = 20.5%, NSG = 6.5%, p = 0.003). However, there is no significant difference in the rate of urosepsis between stenting and URS (SG = 5.7%, NSG = 4.3%, p = 0.681) or after URS (SG = 5.7%, NSG = 2.2%, p = 0.224). The antibiotic prophylaxis strategy for URS (pretreated, standard, targeted) also does not impact urosepsis rates after URS (p = 0.501). Urosepsis in SG is more severe, however, with 40% of SG requiring ICU stay (NSG = 16.7%) and 1 death in SG from urosepsis after URS. The only significant risk factors for developing urosepsis or positive culture check are atherosclerosis (p = 0.012), right sided stents (p = 0.014), and prolonged length of stay (p < 0.001) (Table 1).
Conclusions: Despite sterile ureteral stenting and adequate antibiotic prophylaxis, a significant portion of patients still develop urosepsis or positive culture checks. Surprisingly, this also applies to patients who were initially stented for non-infectious indications. Given the morbidity and mortality of urosepsis, further research to decrease urosepsis rates following URS is needed.
Source of Funding: None.
Methods: We conducted a retrospective cohort study of patients who underwent urgent ureteral stenting followed by URS with laser lithotripsy for urolithiasis management from January 2018 to December 2019 at Northwell Health. Data collected include patient demographics, stent indications, stone characteristics, blood and urine culture results, and antibiotics used. Statistical analyses include Pearson’s Chi Square analysis and Fisher’s Exact test, with p values <0.05 considered statistically significant.
Results: 181 patients were included in this study, with 88 stented for urosepsis concerns (Sepsis Group, SG) and 92 for intractable pain or acute kidney injury (Non-Sepsis Group, NSG). SG is significantly more likely to have a positive culture check (SG = 20.5%, NSG = 6.5%, p = 0.003). However, there is no significant difference in the rate of urosepsis between stenting and URS (SG = 5.7%, NSG = 4.3%, p = 0.681) or after URS (SG = 5.7%, NSG = 2.2%, p = 0.224). The antibiotic prophylaxis strategy for URS (pretreated, standard, targeted) also does not impact urosepsis rates after URS (p = 0.501). Urosepsis in SG is more severe, however, with 40% of SG requiring ICU stay (NSG = 16.7%) and 1 death in SG from urosepsis after URS. The only significant risk factors for developing urosepsis or positive culture check are atherosclerosis (p = 0.012), right sided stents (p = 0.014), and prolonged length of stay (p < 0.001) (Table 1).
Conclusions: Despite sterile ureteral stenting and adequate antibiotic prophylaxis, a significant portion of patients still develop urosepsis or positive culture checks. Surprisingly, this also applies to patients who were initially stented for non-infectious indications. Given the morbidity and mortality of urosepsis, further research to decrease urosepsis rates following URS is needed.
Source of Funding: None.

.jpg)
.jpg)