Back
Poster, Podium & Video Sessions
Podium
PD21: Infections/Inflammation/Cystic Disease of the Genitourinary Tract: Kidney & Bladder II
PD21-09: Identification of key molecular players in the development of Radiation Cystitis through RNA sequencing
Saturday, May 14, 2022
8:20 AM – 8:30 AM
Location: Room 243
Elijah Ward*, Alexander Carabulea, Sarah Bartolone, Laura Lamb, Michael Chancellor, Bernadette Zwaans, Royal Oak, MI
- EW
Podium Presenter(s)
Introduction: Pelvic cancer survivors that were treated with radiation therapy are at risk for developing radiation (hemorrhagic) cystitis (RC) up to 15 years after completion of radiation therapy. Patients with RC suffer from lower urinary tract symptoms, including frequency, nocturia, pelvic pain and incontinence. At an advanced stage, patients can develop hematuria, which can become life-threatening if bleeding cannot be controlled. To date, no safe and reliable therapy exists to treat RC, in part due to the unavailability of bladder biopsies. Taking biopsies of an already fragile bladder is unethical. The objective of this study is to use our established preclinical model to gain insight in the molecular pathways that drive radiation-induced tissue changes in the bladder.
Methods: Female C57Bl/6 mice received a single dose of 40 Gy using the SARRP irradiator. Bladder physiology was assessed using void spot assay. Bladders were harvested at different time points (1 week, 4 weeks, 3 months and 6 months) after irradiation, RNA was harvested, and mRNA sequencing was performed at paired-end 150bp on the Illumina NovaSeq6000 with a target of 30 million reads per sample. Following RNA sequencing, thorough bioinformatics analysis was performed. Findings of the RNA sequencing were validated using qPCR analysis.
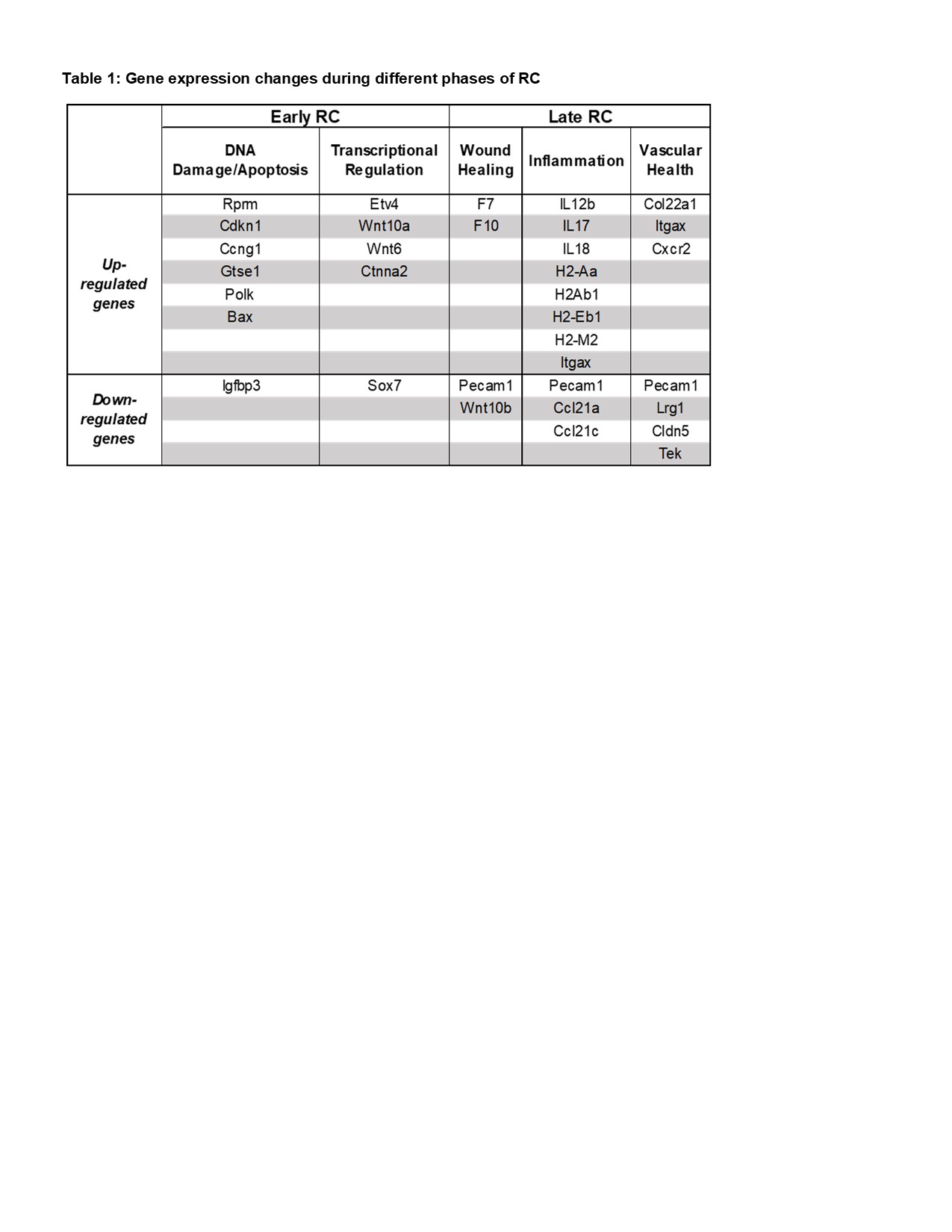
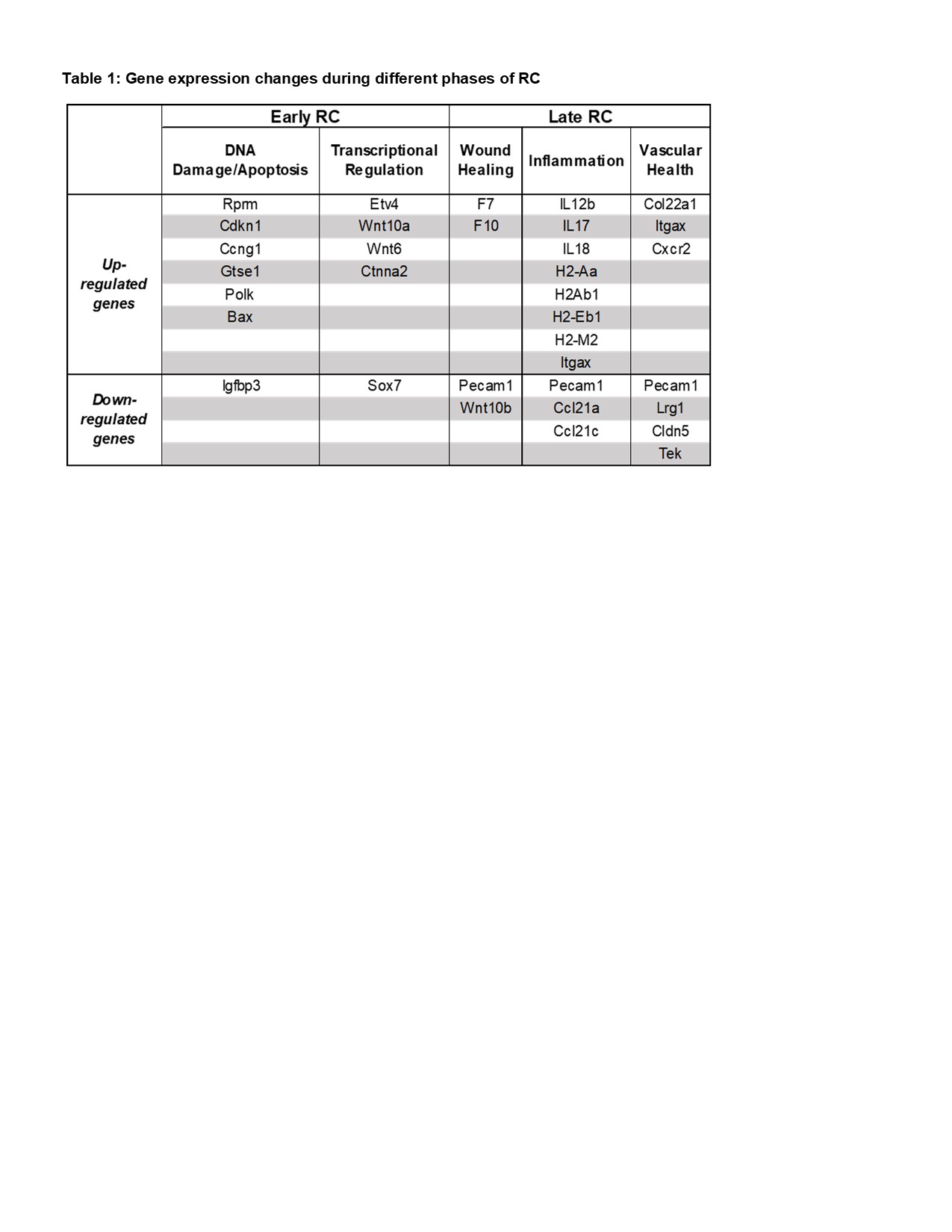
Results: At 1-week post-irradiation, altered gene expression was detected in genes involved in DNA damage response, apoptosis, and transcriptional regulation. By 6-months post-irradiation, significant changes in gene expression were observed in vascular health, wound healing, inflammation, and apoptosis. Genes significantly up- or downregulated in these pathways are listed in table 1. Affected pathways include the Wnt signaling, p53, JAK-STAT, and PI3K-Akt pathways. These findings are currently being validated in vitro in human urothelial cells (SV-HUC-1), and in vivo in bladder tissues from our preclinical model.
Conclusions: The outcome of these studies will have a tremendous impact on the field. This is the first study to determine the molecular changes in the bladder in response to radiation treatment. We hereby identify the physiological changes that drive the progression of radiation cystitis which will aid in identifying potential therapeutic targets.
Source of Funding: This project was in part supported by the NIDDK K01 career development award (BMMZ; DK114334), the U Can-Cer Vive Foundation (BMMZ), and the DMC Foundation.
Methods: Female C57Bl/6 mice received a single dose of 40 Gy using the SARRP irradiator. Bladder physiology was assessed using void spot assay. Bladders were harvested at different time points (1 week, 4 weeks, 3 months and 6 months) after irradiation, RNA was harvested, and mRNA sequencing was performed at paired-end 150bp on the Illumina NovaSeq6000 with a target of 30 million reads per sample. Following RNA sequencing, thorough bioinformatics analysis was performed. Findings of the RNA sequencing were validated using qPCR analysis.
Results: At 1-week post-irradiation, altered gene expression was detected in genes involved in DNA damage response, apoptosis, and transcriptional regulation. By 6-months post-irradiation, significant changes in gene expression were observed in vascular health, wound healing, inflammation, and apoptosis. Genes significantly up- or downregulated in these pathways are listed in table 1. Affected pathways include the Wnt signaling, p53, JAK-STAT, and PI3K-Akt pathways. These findings are currently being validated in vitro in human urothelial cells (SV-HUC-1), and in vivo in bladder tissues from our preclinical model.
Conclusions: The outcome of these studies will have a tremendous impact on the field. This is the first study to determine the molecular changes in the bladder in response to radiation treatment. We hereby identify the physiological changes that drive the progression of radiation cystitis which will aid in identifying potential therapeutic targets.
Source of Funding: This project was in part supported by the NIDDK K01 career development award (BMMZ; DK114334), the U Can-Cer Vive Foundation (BMMZ), and the DMC Foundation.

.jpg)
.jpg)