Back
Poster, Podium & Video Sessions
Podium
PD22: Prostate Cancer: Localized: Radiation Therapy
PD22-02: Restaging Prostate-specific Membrane Antigen Positron Emission Tomography/Computed Tomography is Associated with Improved Oncological Outcome in Men who Underwent Salvage Radiation Therapy for Biochemically Recurrent Prostate Cancer
Saturday, May 14, 2022
9:40 AM – 9:50 AM
Location: Room 252
Dennie Meijer*, Amsterdam, Netherlands, Wietse Eppinga, Utrecht, Netherlands, Roos Mohede, Amsterdam, Netherlands, Ben Vanneste, Maastricht, Netherlands, Philip Meijnen, Otto Meijer, Laurien Daniels, Amsterdam, Netherlands, Roderick Van den Bergh, Nieuwegein, Netherlands, Anne Lont, Amersfoort, Netherlands, Rosemarijn Ettema, Amsterdam, Netherlands, Frederik Oudshoorn, Hoofddorp, Netherlands, Pim van Leeuwen, Henk Van der Poel, Maarten Donswijk, Daniela Oprea-Lager, Eva Schaake, André Vis, Amsterdam, Netherlands
- DM
Podium Presenter(s)
Introduction: Radiolabeled prostate-specific membrane antigen (PSMA)-PET/CT has shown superior diagnostic accuracy for the detection of prostate cancer deposits compared to conventional imaging. Consequently, clinical management changes have been reported in patients with biochemical recurrence (BCR) of disease after robot-assisted radical prostatectomy (RARP). We hypothesized that, due to the exclusion of patients with metastatic disease on PSMA-PET/CT, patients who undergo local salvage radiation therapy (SRT) after restaging PSMA-PET/CT for BCR may have better oncological outcomes than patients who underwent ‘blind’ SRT. Therefore, the aim of this study was to compare the oncological outcome of a patient cohort who underwent PSMA PET-imaging prior to SRT to that of a patient cohort which did not have PSMA PET-imaging before SRT.
Methods: We included 610 patients who underwent SRT, of whom 298 underwent a PSMA-PET/CT prior to SRT, and 312 did not. No additional hormonal therapy was prescribed. To compare both cohorts, case-control matching was performed, using the prostate-specific antigen (PSA)-value at initiation of SRT, pathological Grade Group, pathological T-stage, surgical margin status, and biochemical persistence after RARP as matching variables. Outcome variable was biochemical progression at one year after SRT, defined as either a rise of PSA =0.2 ng/mL above the nadir after SRT, or the start of additional treatment.
Results: After case-control matching, 216 patients were matched in both cohorts (108 patients per cohort). In the patient cohort without PSMA-PET/CT prior to SRT, 23/108 patients (21%) had biochemical progression of disease at one year after SRT, compared to 9/108 patients (8%) who underwent restaging PSMA-PET/CT prior to SRT (p=0.007).
Conclusions: Patients who underwent restaging PSMA-PET/CT for BCR after RARP had better short-term oncological outcomes after SRT than those who underwent ‘blind’ SRT. Thus, PSMA-PET/CT is associated with an improved oncological outcome in a selected series of patients.
Source of Funding: None
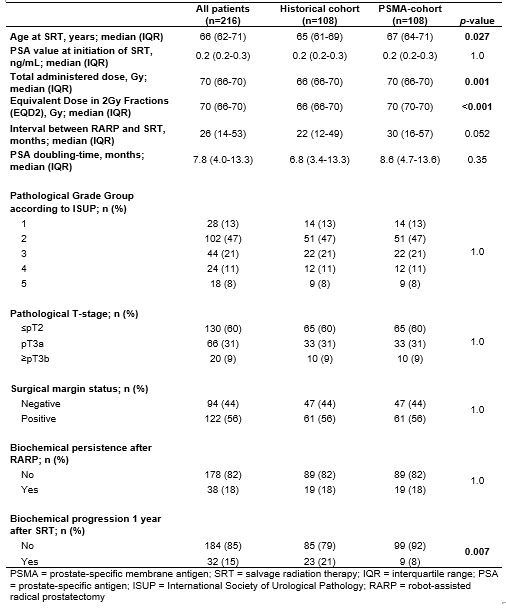
Methods: We included 610 patients who underwent SRT, of whom 298 underwent a PSMA-PET/CT prior to SRT, and 312 did not. No additional hormonal therapy was prescribed. To compare both cohorts, case-control matching was performed, using the prostate-specific antigen (PSA)-value at initiation of SRT, pathological Grade Group, pathological T-stage, surgical margin status, and biochemical persistence after RARP as matching variables. Outcome variable was biochemical progression at one year after SRT, defined as either a rise of PSA =0.2 ng/mL above the nadir after SRT, or the start of additional treatment.
Results: After case-control matching, 216 patients were matched in both cohorts (108 patients per cohort). In the patient cohort without PSMA-PET/CT prior to SRT, 23/108 patients (21%) had biochemical progression of disease at one year after SRT, compared to 9/108 patients (8%) who underwent restaging PSMA-PET/CT prior to SRT (p=0.007).
Conclusions: Patients who underwent restaging PSMA-PET/CT for BCR after RARP had better short-term oncological outcomes after SRT than those who underwent ‘blind’ SRT. Thus, PSMA-PET/CT is associated with an improved oncological outcome in a selected series of patients.
Source of Funding: None

.jpg)
.jpg)