Back
Poster, Podium & Video Sessions
Podium
PD29: Trauma/Reconstruction/Diversion: External Genitalia Reconstruction and Urotrauma (including transgender surgery) II
PD29-11: Intra-abdominal complications following peritoneal flap vaginoplasty
Saturday, May 14, 2022
2:40 PM – 2:50 PM
Location: Room 244
Isabel Robinson*, Rachel Bluebond-Langner, Lee Zhao, New York, NY
- IR
Podium Presenter(s)
Introduction: The peritoneal flap vaginoplasty is a technique for achieving substantial neovaginal depth. Intra-abdominal complications following robotic peritoneal flap creation are rare but prompt diagnosis and management is critical to preventing patient harm. The purpose of this study was to describe the authors’ experience with managing intra-abdominal complications following peritoneal flap vaginoplasty.
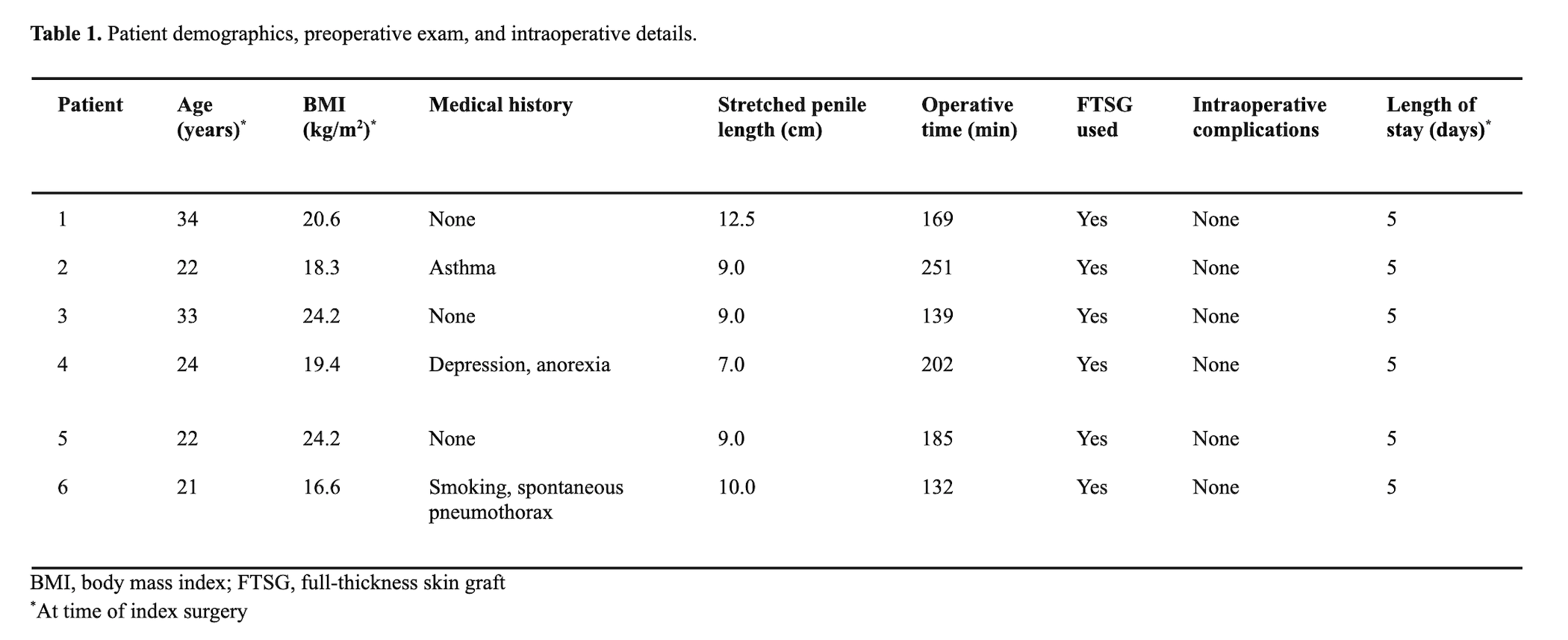
Methods: Retrospective chart review identified patients undergoing robotically assisted peritoneal flap vaginoplasty by the senior authors between 2017 and 2020 who subsequently developed intra-abdominal complications requiring readmission and/or return to the operating room. Patient charts were analyzed for preoperative demographics, medical comorbidities, intraoperative details, postoperative complication presentation, diagnosis, management, and long-term outcomes.
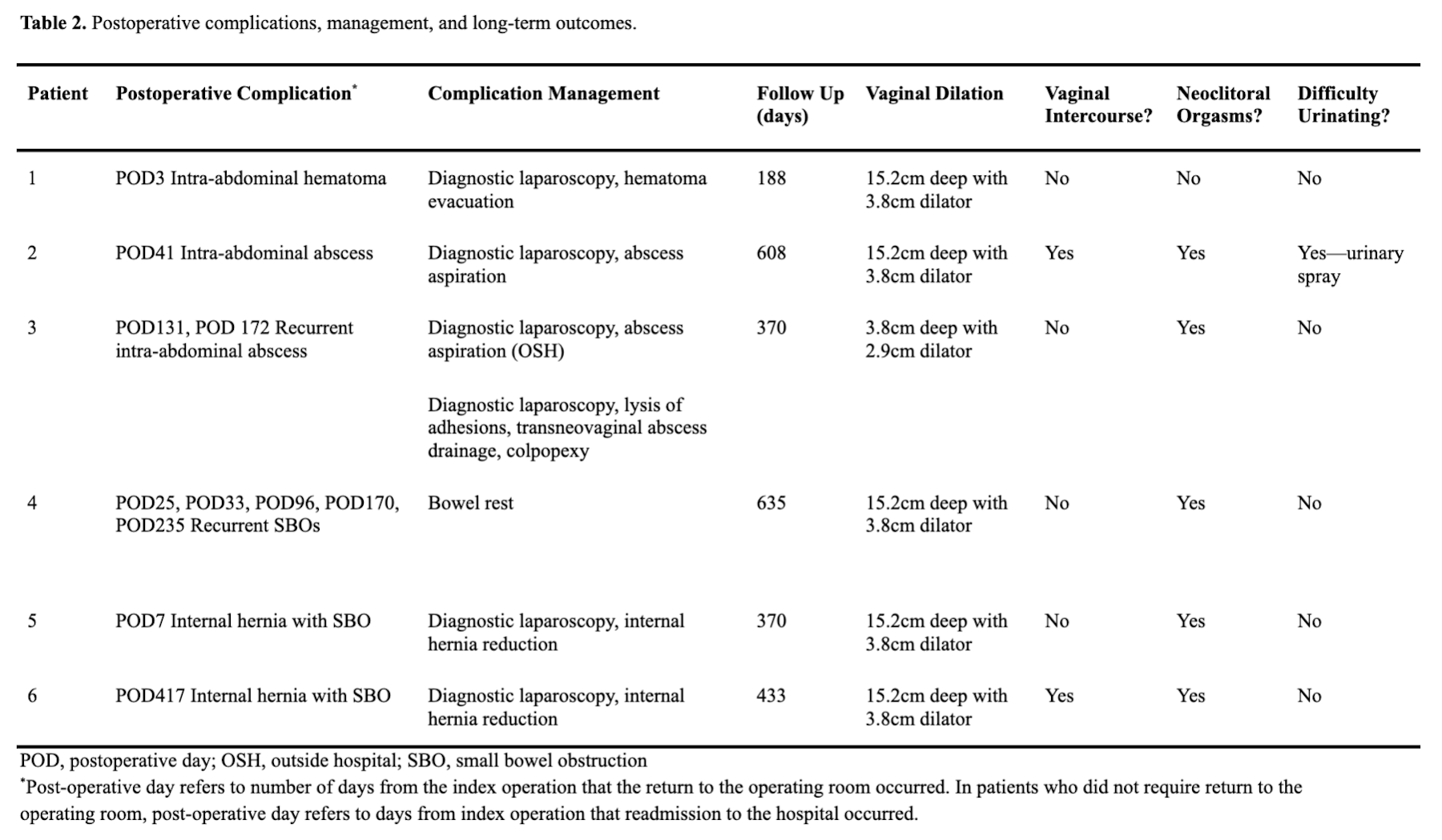
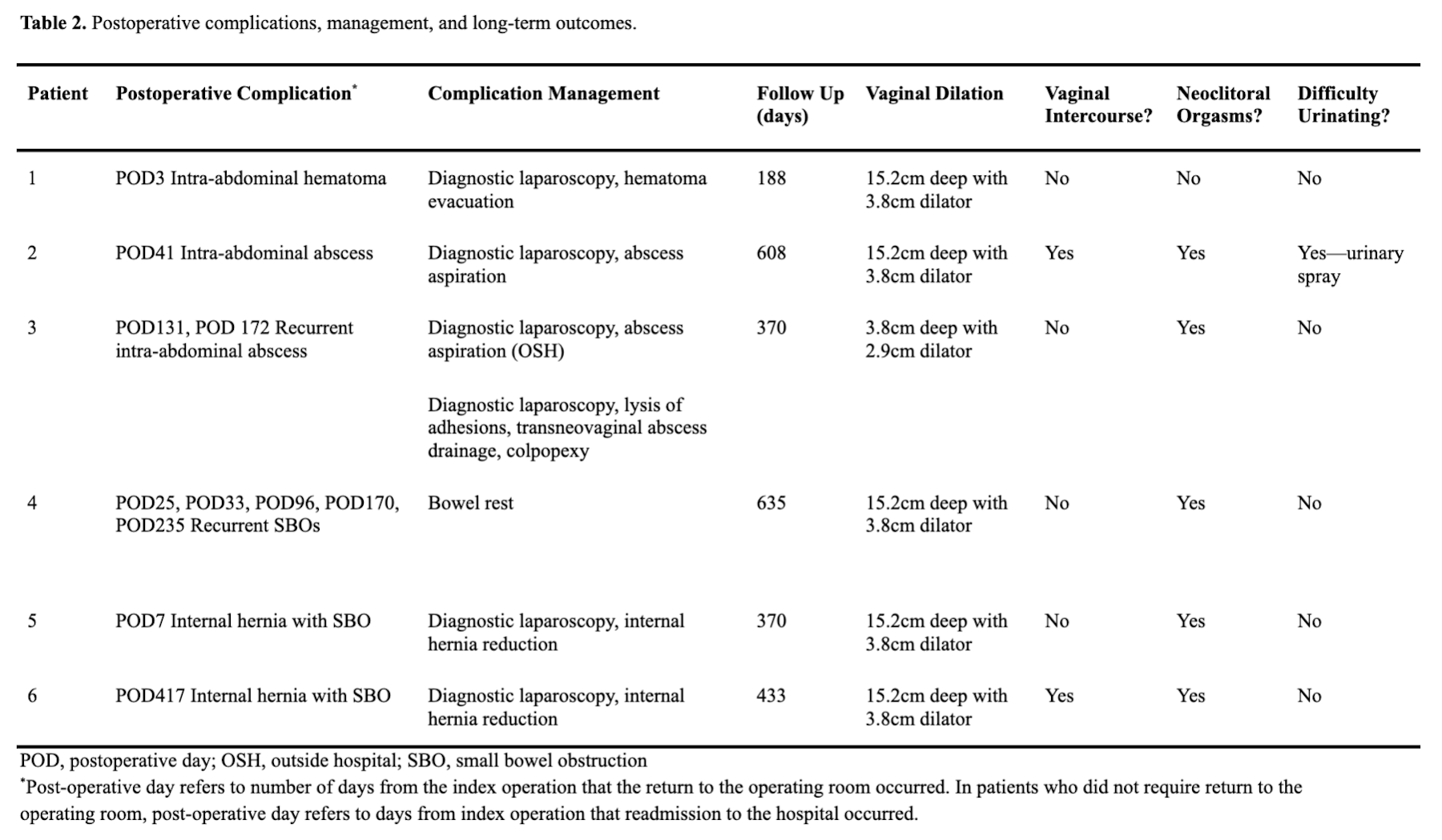
Results: Out of 274 patients undergoing peritoneal flap vaginoplasty during the study period, six patients were identified who developed intra-abdominal complications (2.2%). One patient developed postoperative hematoma requiring return to the operating room for diagnostic laparoscopy and hematoma evacuation. Two patient developed intraabdominal abscesses requiring diagnostic laparoscopy and abscess drainage. One patient developed recurrent episodes of small bowel obstructions that resolved with bowel rest. Two patients developed incarcerated internal hernias requiring diagnostic laparoscopy and internal hernia reduction. In one case, the hernia occurred at the peritoneal flap closure site, and in the other care the hernia occurred at the peritoneal flap donor site.
Conclusions: Intra-abdominal complications following robot assisted peritoneal flap vaginoplasty require prompt surgical attention. In addition to hematoma and abscess, small bowel incarceration and internal hernias are important complications for the surgeon performing peritoneal flap vaginoplasty to consider.
Source of Funding: N/A
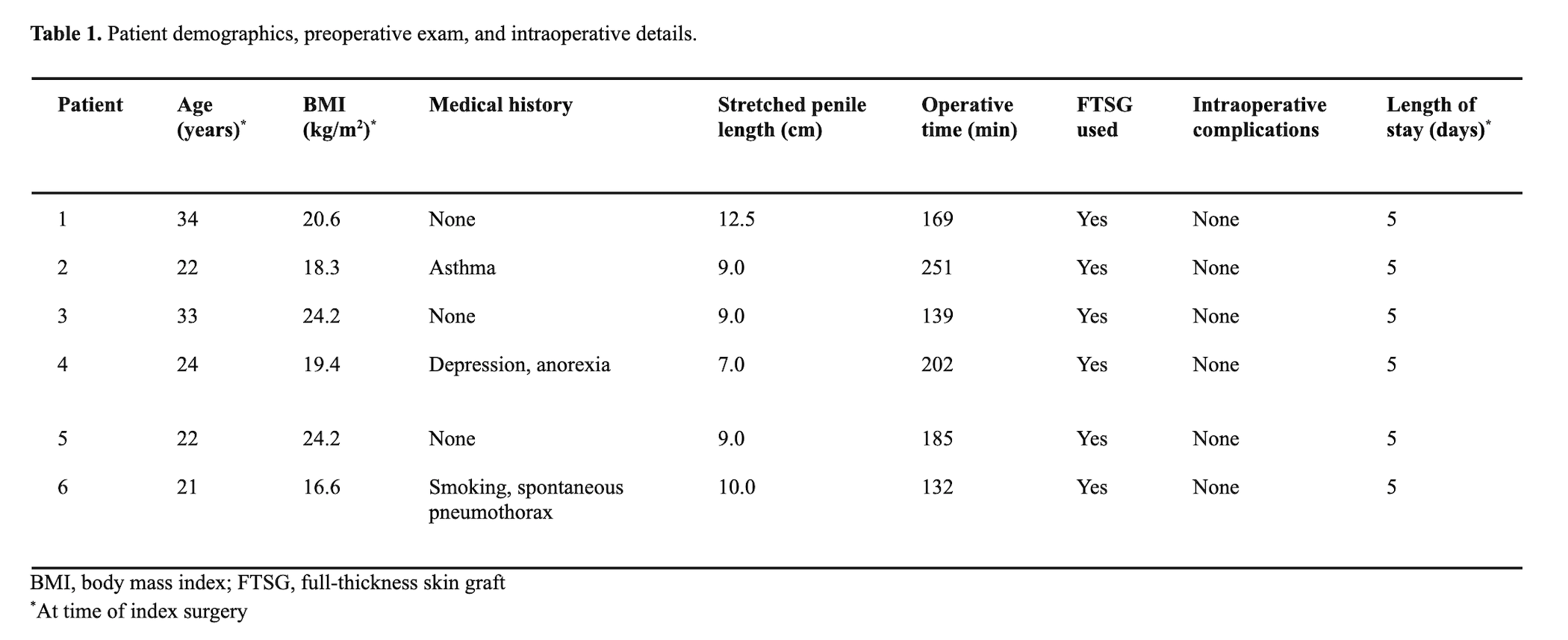
Methods: Retrospective chart review identified patients undergoing robotically assisted peritoneal flap vaginoplasty by the senior authors between 2017 and 2020 who subsequently developed intra-abdominal complications requiring readmission and/or return to the operating room. Patient charts were analyzed for preoperative demographics, medical comorbidities, intraoperative details, postoperative complication presentation, diagnosis, management, and long-term outcomes.
Results: Out of 274 patients undergoing peritoneal flap vaginoplasty during the study period, six patients were identified who developed intra-abdominal complications (2.2%). One patient developed postoperative hematoma requiring return to the operating room for diagnostic laparoscopy and hematoma evacuation. Two patient developed intraabdominal abscesses requiring diagnostic laparoscopy and abscess drainage. One patient developed recurrent episodes of small bowel obstructions that resolved with bowel rest. Two patients developed incarcerated internal hernias requiring diagnostic laparoscopy and internal hernia reduction. In one case, the hernia occurred at the peritoneal flap closure site, and in the other care the hernia occurred at the peritoneal flap donor site.
Conclusions: Intra-abdominal complications following robot assisted peritoneal flap vaginoplasty require prompt surgical attention. In addition to hematoma and abscess, small bowel incarceration and internal hernias are important complications for the surgeon performing peritoneal flap vaginoplasty to consider.
Source of Funding: N/A

.jpg)
.jpg)