Back
Poster, Podium & Video Sessions
Podium
PD31: Trauma/Reconstruction/Diversion: Urethral Reconstruction (including Stricture, Diverticulum) II
PD31-11: Patient, Stricture, and Urethroplasty Predictors of Erectile Dysfunction after Urethroplasty for Bulbar Urethral Strictures
Saturday, May 14, 2022
5:10 PM – 5:20 PM
Location: Room 252
Justin Drobish*, Iowa City, IA, Shawn Grove, Minneapolis, MN, Nejd Alsikafi, Gurnee, IL, Joshua Broghammer, Kansas City, KS, Jill Buckley, San Diego, CA, Sean Elliott, Minneapolis, MN, Jeremy Myers, Salt Lake City, UT, Andrew Peterson, Durham , NC, Keith Rourke, Edmonton , Canada, Thomas Smith III, Houston, TX, Alex Vanni, Burlington, MA, Lee Zhao, New York City, NY, Bradley Erickson, Iowa City, IA

Justin N. Drobish, MD
University of Iowa Hospitals and Clinics
Podium Presenter(s)
Introduction: Bulbar urethroplasty (BU) for urethral stricture disease can significantly improve urinary quality of life (QOL). However, prior studies have shown that while erectile dysfunction (ED) is rare, its presence after BU negatively affects QOL and satisfaction regardless of stricture outcome. Herein we analyze patient, stricture and urethroplasty variables and their association with post-BU ED.
Methods: The Trauma and Urologic Reconstruction Network of Surgeons (TURNS) prospective database was used to create a cohort of bulbar (S1a/S1b; no posterior or penile urethral extension) urethral strictures that underwent single-stage BU from 2010 to 2018 with minimum 3-year clinical follow-up (database + retrospective chart review) not associated with hypospadias. Patient, stricture, and repair variables were analyzed for their association with ED, which was determined with retrospective chart review of both urologic and non-urologic clinical visits in the 12 months after BU, looking for patient complaints of ED and/or new prescriptions for ED medications, with uni- and multivariable models. Patient-reported recovery of erectile function was also assessed with chart review.
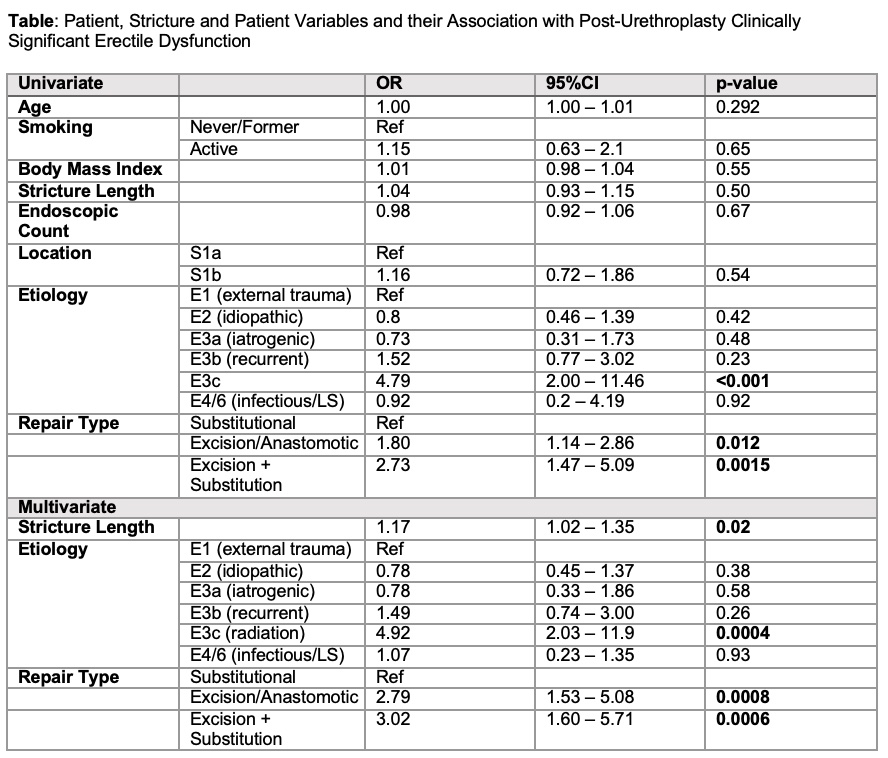
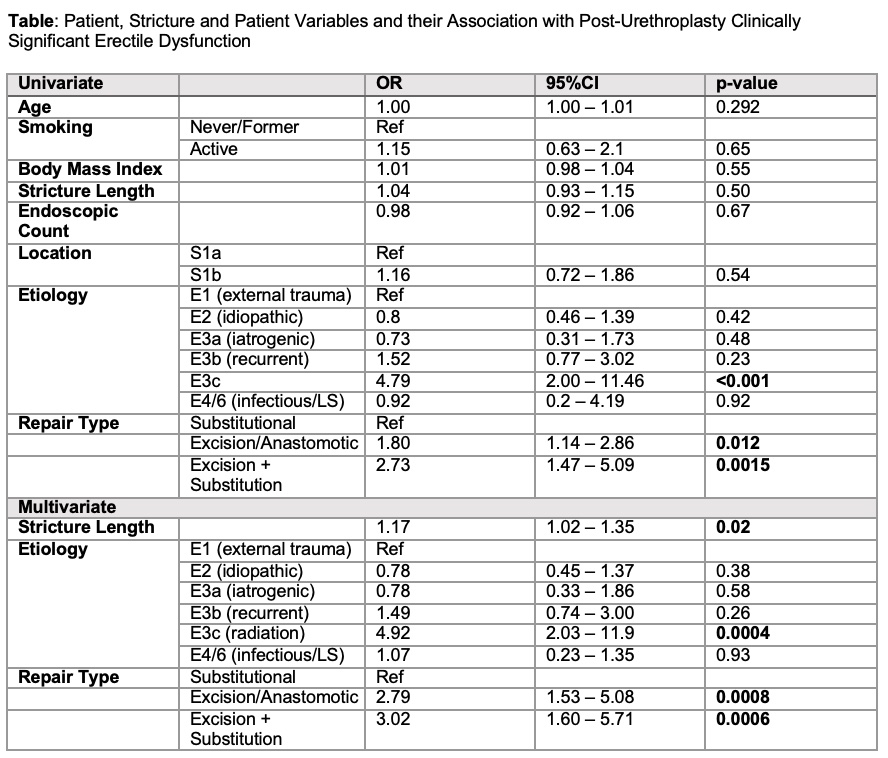
Results: At a median follow-up time was 65.1 months, 108 (7.3%) of 1480 study subjects were noted to have clinically significant post-BU ED. Uni- and multivariate predictors of post-BU ED are shown in the Table. On multivariate analysis, a history of pelvic radiation and BU involving urethral excision/transection significantly increased the odds of ED. Recovery of function was confirmed 56 (51.9%) at a median follow-up of 19 mo. and was not affected by repair type.
Conclusions: Clinically significant changes in erectile function occurs in at least 7% of BU cases, with urethral excision/transection and radiation history significantly increasing the odds. Notably, traditional patient factors associated with ED, including as age, BMI and smoking history, did not affect the development of de novo post-BU ED. Most, but not all, patients appear to recover with time.
Source of Funding: NIDDK 1R21DK115945-01
Methods: The Trauma and Urologic Reconstruction Network of Surgeons (TURNS) prospective database was used to create a cohort of bulbar (S1a/S1b; no posterior or penile urethral extension) urethral strictures that underwent single-stage BU from 2010 to 2018 with minimum 3-year clinical follow-up (database + retrospective chart review) not associated with hypospadias. Patient, stricture, and repair variables were analyzed for their association with ED, which was determined with retrospective chart review of both urologic and non-urologic clinical visits in the 12 months after BU, looking for patient complaints of ED and/or new prescriptions for ED medications, with uni- and multivariable models. Patient-reported recovery of erectile function was also assessed with chart review.
Results: At a median follow-up time was 65.1 months, 108 (7.3%) of 1480 study subjects were noted to have clinically significant post-BU ED. Uni- and multivariate predictors of post-BU ED are shown in the Table. On multivariate analysis, a history of pelvic radiation and BU involving urethral excision/transection significantly increased the odds of ED. Recovery of function was confirmed 56 (51.9%) at a median follow-up of 19 mo. and was not affected by repair type.
Conclusions: Clinically significant changes in erectile function occurs in at least 7% of BU cases, with urethral excision/transection and radiation history significantly increasing the odds. Notably, traditional patient factors associated with ED, including as age, BMI and smoking history, did not affect the development of de novo post-BU ED. Most, but not all, patients appear to recover with time.
Source of Funding: NIDDK 1R21DK115945-01

.jpg)
.jpg)