Back
Poster, Podium & Video Sessions
Podium
PD33: Kidney Cancer: Localized: Surgical Therapy II
PD33-06: Split Renal Function Improves Prediction of GFR after Radical Nephrectomy
Saturday, May 14, 2022
4:10 PM – 4:20 PM
Location: Room 245
Nityam Rathi*, Yosuke Yasuda, Diego Aguilar Palacios, Cleveland, OH, Hajime Tanaka, Tokyo, Japan, Yunlin Ye, Guangzhou, China, People's Republic of, Jianbo Li, Cleveland, OH, Bimal Bhindi, Calgary, Canada, Robert Houston, Rochester, MN, Michael Liss, San Antonio, TX, Ithaar Derweesh, La Jolla, CA, Christopher Weight, Mohammed Eltemamy, Robert Abouassaly, Steven Campbell, Cleveland, OH
.jpg)
Nityam Rathi, BS (he/him/his)
Cleveland Clinic
Podium Presenter(s)
Introduction: While partial nephrectomy (PN) is the preferred surgical option in renal cell carcinoma (RCC) due to better functional outcomes, radical nephrectomy (RN) is relevant in cases of increased oncologic potential. Studies suggest that patients with new baseline GFR (NBGFR) > 45ml/min/1.73m2 after RN/PN have strong survival outcomes. Thus, predicting NBGFR after RN has significant clinical implications for RCC management, including complex decisions about RN/PN. Predicting NBGFR post-RN has proven to be challenging, perhaps due to omission of two important functional parameters: split renal function (SRF) and renal functional compensation (RFC) in the contralateral kidney. We compare the predictive accuracy of our SRF-based model against published non-SRF-based models.
Methods: All 445 RCC patients who underwent RN (2010-14) with preoperative CT/MRI and relevant preop/postoperative GFR estimations were analyzed. SRF was determined using semi-automated software that provides differential parenchymal volume analysis (PVA) from preoperative imaging (FUJIFILM Medical Systems). NBGFR was defined as GFR 3-12 months after RN, and RFC was estimated at 24% from independent analysis. Our SRF-based model was: Predicted NBGFR = 1.24 × Global GFRPre-RN × SRF1. Five published non-SRF-based models were also assessed on the same cohort2-6. Predictive accuracy of each model was assessed by the correlation coefficient (r).
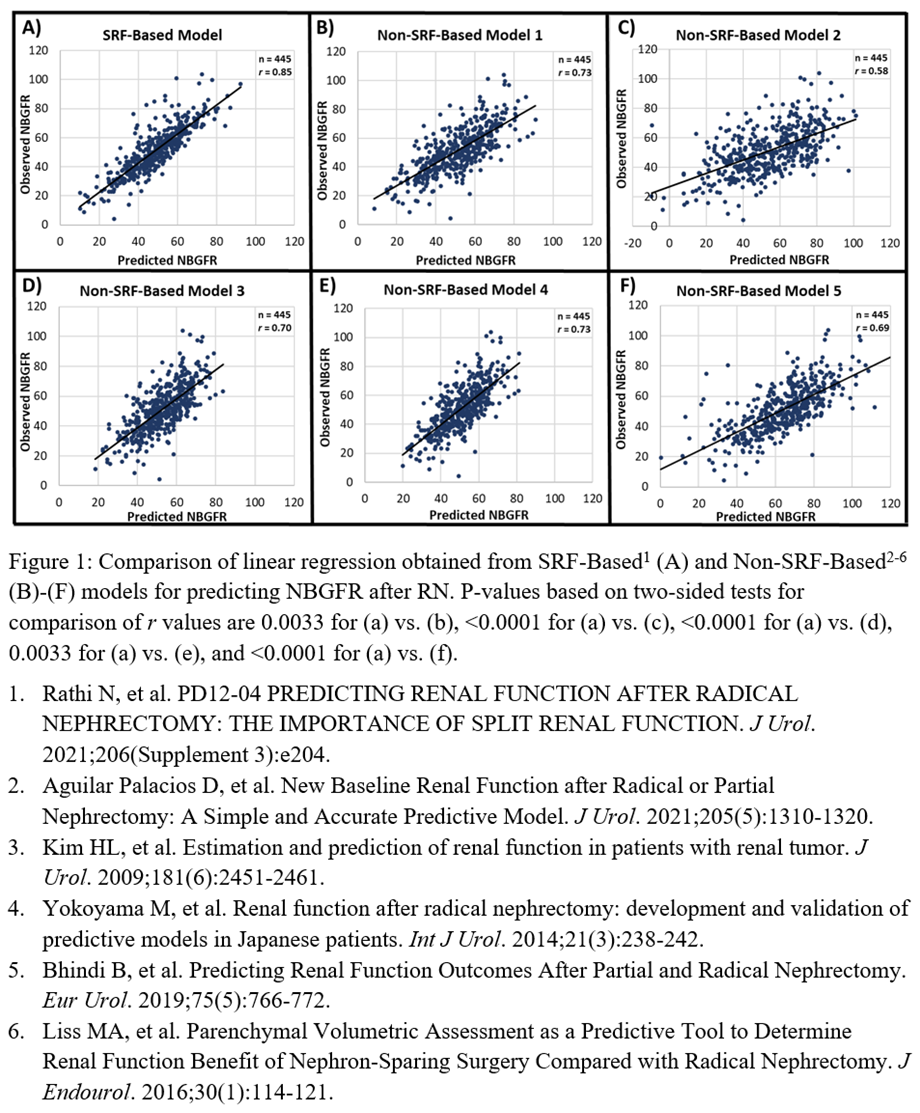
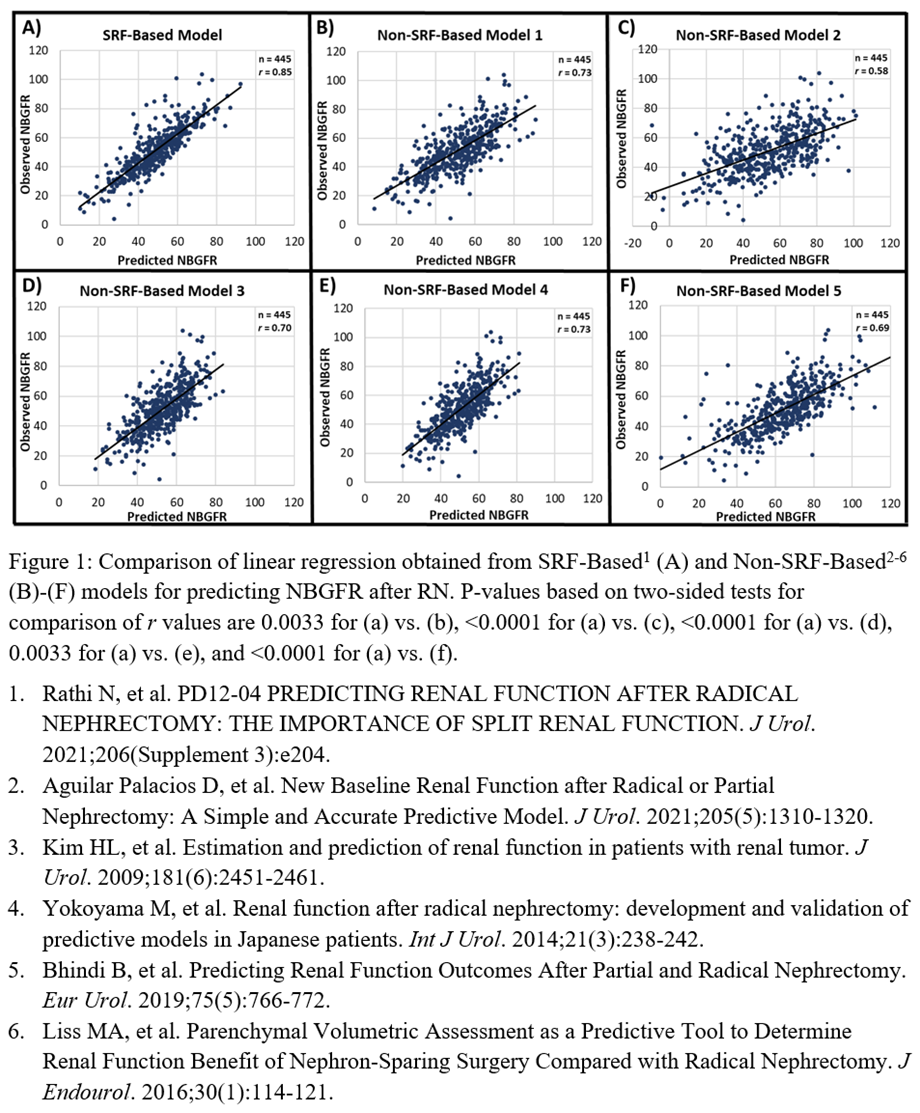
Results: The r value for the SRF-based model was 0.85 (Figure 1A). The r values for the non-SRF-based models were 0.73, 0.58, 0.70, 0.73, and 0.69 (Figure 1B-F, respectively). Differences in r for the SRF-based model and non-SRF-based models were all statistically significant (p < 0.005).
Conclusions: A conceptually simple model based on preoperative SRF and RFC more accurately predicts NBGFR after RN than non-SRF-based models, which are more complex. The SRF-based model relies on preoperative imaging and labs that patients routinely receive. SRF can be determined using readily available PVA software, which is inexpensive and more accurate than nuclear renal scans, thereby enhancing the practicality of our approach. Clinically, the SRF-based model can be used to facilitate complex decisions regarding PN/RN for RCC and other imperative conditions.
Source of Funding: None
Methods: All 445 RCC patients who underwent RN (2010-14) with preoperative CT/MRI and relevant preop/postoperative GFR estimations were analyzed. SRF was determined using semi-automated software that provides differential parenchymal volume analysis (PVA) from preoperative imaging (FUJIFILM Medical Systems). NBGFR was defined as GFR 3-12 months after RN, and RFC was estimated at 24% from independent analysis. Our SRF-based model was: Predicted NBGFR = 1.24 × Global GFRPre-RN × SRF1. Five published non-SRF-based models were also assessed on the same cohort2-6. Predictive accuracy of each model was assessed by the correlation coefficient (r).
Results: The r value for the SRF-based model was 0.85 (Figure 1A). The r values for the non-SRF-based models were 0.73, 0.58, 0.70, 0.73, and 0.69 (Figure 1B-F, respectively). Differences in r for the SRF-based model and non-SRF-based models were all statistically significant (p < 0.005).
Conclusions: A conceptually simple model based on preoperative SRF and RFC more accurately predicts NBGFR after RN than non-SRF-based models, which are more complex. The SRF-based model relies on preoperative imaging and labs that patients routinely receive. SRF can be determined using readily available PVA software, which is inexpensive and more accurate than nuclear renal scans, thereby enhancing the practicality of our approach. Clinically, the SRF-based model can be used to facilitate complex decisions regarding PN/RN for RCC and other imperative conditions.
Source of Funding: None

.jpg)
.jpg)