Back
Poster, Podium & Video Sessions
Podium
PD34: Urodynamics/Lower Urinary Tract Dysfunction/Female Pelvic Medicine: Female Incontinence: Therapy II
PD34-05: Does Cognitive Impairment Impact Sacral Neuromodulation in Older Patients with Overactive Bladder?
Saturday, May 14, 2022
4:10 PM – 4:20 PM
Location: Room 244
Jacqueline Zillioux*, Kevin Lewis, Daniel Hettel, Sarah Martin, Lauren Gleich, Howard B. Goldman, Bradley Gill, Cleveland, OH

Jacqueline Zillioux, MD
Cleveland Clinic
Podium Presenter(s)
Introduction: Overactive bladder (OAB) and cognitive impairment (CI) are both increasingly prevalent with age. Given the association between anticholinergics and dementia, there is need to optimize other therapies. Though AUA/SUFU OAB guidelines cite intact cognitive ability as necessary to maintain sacral neuromodulation (SNM), the impact of cognitive function on SNM outcomes remains unknown. This study assessed the impact of CI diagnosis on SNM in older patients.
Methods: A retrospective review was completed of patients =55 years old who underwent test-phase SNM (peripheral nerve evaluation (PNE) or stage 1) for urge-frequency or urgency urinary incontinence between 1/2014-3/2021 within a large regional health system. Patient demographics, comorbidities, CI diagnoses (dementia or mild CI), OAB medication and/or botulinum toxin use, and SNM procedures were recorded. SNM procedures and outcomes were categorized as implant, explant, and/or revision. Uni- and multivariable logistic regression modeling assessed for the impact of CI on implantation rates.
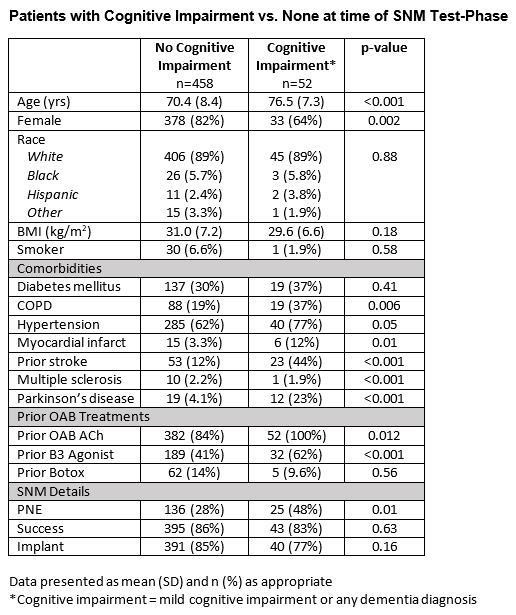
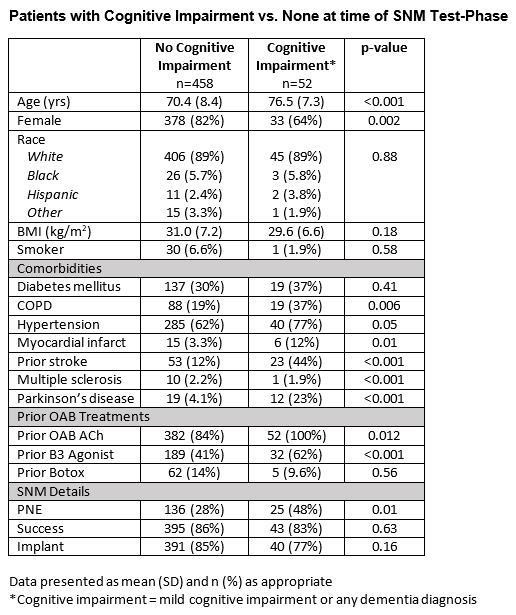
Results: A total of 510 patients underwent SNM test-phase (161 PNE, 349 Stage 1). Mean age was 71.0 (8.5) years and the majority (79.6%) were female. Overall, 52 (10.1%) patients had a CI diagnosis at the time of SNM, and 30 (6.0%) were diagnosed after SNM at a median 18.5 [9.25, 39.5] months. Patients with CI were older with more comorbidities and were more likely to undergo PNE (Table 1). Univariable analysis found no difference in implantation rate based on pre-SNM CI (85.4% vs 76.9%, p=0.16). Multivariable modeling identified PNE (OR 0.42, 95%CI 0.26-0.70) and age (OR 0.95, 95%CI 0.93-0.98), but not CI or dementia, as independent negative predictors of implantation. Implanted patients had median follow-up of 12 [4.0, 39.5] months. Patients with CI were more likely to continue B3 agonists (37.1% vs 16.0%, p=0.04) following implant but rates of anticholinergic or new intradetrusor botulinum toxin use did not differ. Explant (12.1%), revision (10.4%), and battery replacement (3.4%) rates also did not differ according to CI.
Conclusions: Patients with CI and OAB proceed to SNM implant at rates that do not differ from patients without cognitive deficits. CI should not preclude providers from offering SNM for refractory OAB.
Source of Funding: NA
Methods: A retrospective review was completed of patients =55 years old who underwent test-phase SNM (peripheral nerve evaluation (PNE) or stage 1) for urge-frequency or urgency urinary incontinence between 1/2014-3/2021 within a large regional health system. Patient demographics, comorbidities, CI diagnoses (dementia or mild CI), OAB medication and/or botulinum toxin use, and SNM procedures were recorded. SNM procedures and outcomes were categorized as implant, explant, and/or revision. Uni- and multivariable logistic regression modeling assessed for the impact of CI on implantation rates.
Results: A total of 510 patients underwent SNM test-phase (161 PNE, 349 Stage 1). Mean age was 71.0 (8.5) years and the majority (79.6%) were female. Overall, 52 (10.1%) patients had a CI diagnosis at the time of SNM, and 30 (6.0%) were diagnosed after SNM at a median 18.5 [9.25, 39.5] months. Patients with CI were older with more comorbidities and were more likely to undergo PNE (Table 1). Univariable analysis found no difference in implantation rate based on pre-SNM CI (85.4% vs 76.9%, p=0.16). Multivariable modeling identified PNE (OR 0.42, 95%CI 0.26-0.70) and age (OR 0.95, 95%CI 0.93-0.98), but not CI or dementia, as independent negative predictors of implantation. Implanted patients had median follow-up of 12 [4.0, 39.5] months. Patients with CI were more likely to continue B3 agonists (37.1% vs 16.0%, p=0.04) following implant but rates of anticholinergic or new intradetrusor botulinum toxin use did not differ. Explant (12.1%), revision (10.4%), and battery replacement (3.4%) rates also did not differ according to CI.
Conclusions: Patients with CI and OAB proceed to SNM implant at rates that do not differ from patients without cognitive deficits. CI should not preclude providers from offering SNM for refractory OAB.
Source of Funding: NA

.jpg)
.jpg)