Back
Poster, Podium & Video Sessions
Podium
PD35: Prostate Cancer: Advanced (including Drug Therapy) II
PD35-02: When Is Neoadjuvant Androgen Deprivation Therapy Beneficial for Highly Aggressive Prostate Cancer Candidates to Radical Prostatectomy? Implications for Multi-modal Tailored Approaches and Trials Design
Sunday, May 15, 2022
7:10 AM – 7:20 AM
Location: Room 252
Francesco Barletta*, Giorgio Gandaglia, Simone Scuderi, Giuseppe Ottone Cirulli, Elio Mazzone, Milano, Italy, Armando Stabile, Milan, Italy, Andrea Necchi, Laura Marandino, Daniele Raggi, Milano, Italy, Vito Cucchiara, Milan, Italy, Daniele Robesti, Milano, Italy, Emanuele Zaffuto, Luigi Nocera, Milan, Italy, Donato Cannoletta, Milano, Italy, Mario De Angelis, Milan, Italy, Pierre I. Karakiewicz, Montreal, Canada, Francesco Montorsi, Alberto Briganti, Milano, Italy
- FB
Podium Presenter(s)
Introduction: A revitalized interest on neoadjuvant androgen deprivation therapy (ADT) in prostate cancer (PCa) has been raised by the introduction of novel androgen receptor targeting agents. Identifying men who might benefit from neoadjuvant hormonal manipulation is key for both tailored approaches and for selecting the proper population to include in trials testing new neo-adjuvant therapies.
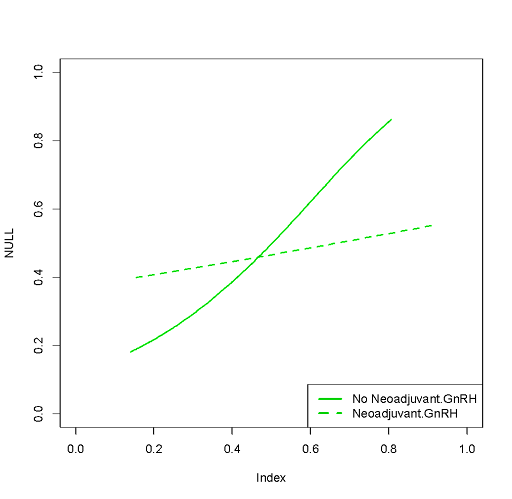
Methods: We evaluated 411 patients with biopsy GG5 PCa treated with radical prostatectomy (RP) with an extended pelvic lymph node dissection (PLND) between 1995 and 2021. Neoadjuvant or adjuvant treatments (namely, ADT and/or radiotherapy) were administered according to the treating physician’s preference. Biochemical recurrence (BCR) was defined as two PSA values >0.2 ng/ml. Clinical recurrence (CR) was the onset of metastases at conventional imaging. An interaction test assessed whether the impact of the neoadjuvant ADT varied according to a risk score based on preoperative features and developed in men who received RP alone. The observed vs. predicted CR-free survival was plotted for neoadjuvant ADT vs. no neoadjuvant ADT.
Results: Median PSA was 10 ng/ml. Overall, 149 (36%) and 55 (14%) patients had cT3 at DRE and cN1 at conventional imaging. Overall, 95 (23%), 161 (40%), and 219 (53%) men received neoadjuvant, adjuvant ADT and/or radiotherapy. A total of 140 (34%) patients received RP alone. The median number of nodes removed was 21. Overall, 238 (58%), 210 (51%) and 179 (44%) patients had pT3b, pN1 and positive margins. Neoadjuvant ADT was associated with lower risk of PSM (33 vs. 48%, p=0.001). Median follow-up was 61 months and 106 men experienced CR. The 7-year CR-free survival rate was 61%. A cT3 (HR: 2.22; p=0.01) and higher PSA (HR: 1.01; p=0.01) predicted CR at multivariable analyses. The impact of neoadjuvant ADT on CR-free survival varied according to a risk score based on cT3, PSA and cN. Men with a risk of CR higher than 40% at 8-year according to the risk score are those who benefit from upfront ADT.
Conclusions: Neoadjuvant ADT might be highly beneficial in patients with biopsy GG5 PCa with aggressive disease characteristics. This should guide the selection of trial populations in this setting.
Source of Funding: .
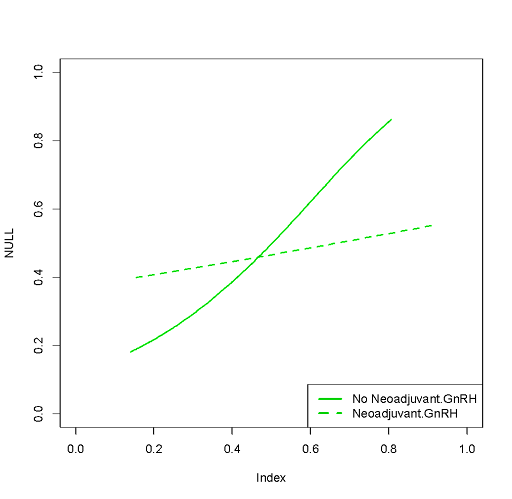
Methods: We evaluated 411 patients with biopsy GG5 PCa treated with radical prostatectomy (RP) with an extended pelvic lymph node dissection (PLND) between 1995 and 2021. Neoadjuvant or adjuvant treatments (namely, ADT and/or radiotherapy) were administered according to the treating physician’s preference. Biochemical recurrence (BCR) was defined as two PSA values >0.2 ng/ml. Clinical recurrence (CR) was the onset of metastases at conventional imaging. An interaction test assessed whether the impact of the neoadjuvant ADT varied according to a risk score based on preoperative features and developed in men who received RP alone. The observed vs. predicted CR-free survival was plotted for neoadjuvant ADT vs. no neoadjuvant ADT.
Results: Median PSA was 10 ng/ml. Overall, 149 (36%) and 55 (14%) patients had cT3 at DRE and cN1 at conventional imaging. Overall, 95 (23%), 161 (40%), and 219 (53%) men received neoadjuvant, adjuvant ADT and/or radiotherapy. A total of 140 (34%) patients received RP alone. The median number of nodes removed was 21. Overall, 238 (58%), 210 (51%) and 179 (44%) patients had pT3b, pN1 and positive margins. Neoadjuvant ADT was associated with lower risk of PSM (33 vs. 48%, p=0.001). Median follow-up was 61 months and 106 men experienced CR. The 7-year CR-free survival rate was 61%. A cT3 (HR: 2.22; p=0.01) and higher PSA (HR: 1.01; p=0.01) predicted CR at multivariable analyses. The impact of neoadjuvant ADT on CR-free survival varied according to a risk score based on cT3, PSA and cN. Men with a risk of CR higher than 40% at 8-year according to the risk score are those who benefit from upfront ADT.
Conclusions: Neoadjuvant ADT might be highly beneficial in patients with biopsy GG5 PCa with aggressive disease characteristics. This should guide the selection of trial populations in this setting.
Source of Funding: .

.jpg)
.jpg)