Back
Poster, Podium & Video Sessions
Podium
PD38: Urodynamics/Lower Urinary Tract Dysfunction/Female Pelvic Medicine: Non-neurogenic Voiding Dysfunction II
PD38-07: High Flow Bladder Outlet Obstruction in Men
Sunday, May 15, 2022
8:00 AM – 8:10 AM
Location: Room 244
Aaron Huang*, Brooklyn, NY, Kevin Rychik, Tel-Aviv, Israel, Max Edeson, Nutley, NJ, Wade Bushman, Madison, WI, Jerry Blaivas, New York, NY

Aaron Huang, BA
SUNY Downstate Health Sciences University
Podium Presenter(s)
Introduction: High flow bladder outlet obstruction (HF BOO) was first coined in 1982 describing patients with a normal maximum flow rate (Qmax) of =15 mL/s, but with BOO defined by the bladder outlet obstruction index (BOOI). HF BOO is a subset of BOO for which there are no established treatment guidelines. Uroflowmetry is well-established as a screening test for BOO and for those with a Qmax = 15 mL/s, BOO is thought to be “ruled out.” The objective of this study is to highlight the prevalence of HF BOO in males and the clinical implications of this diagnosis.
Methods: This was a retrospective review of an ongoing database of men with refractory lower urinary tract symptoms (LUTS) who underwent videourodynamic studies (VUDS). Patient demographics and urodynamics data were collected, and those with incomplete data or erroneous urodynamic tracings were excluded. Patients were diagnosed with BOO if the BOOI > 40 and HF BOO if a contemporaneous pressure or free-flow Qmax = 15 mL/s. A two-tailed independent sample t-test was conducted to compare urodynamic parameters between men with BOO and men with HF BOO. For HF BOO patients, post-treatment free-flow values were compared when treated conservatively and surgically.
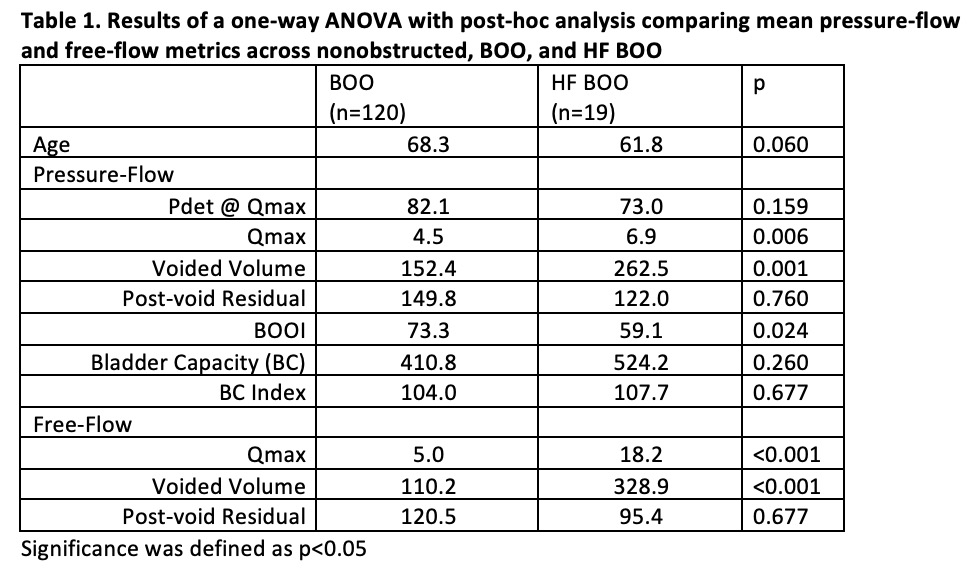
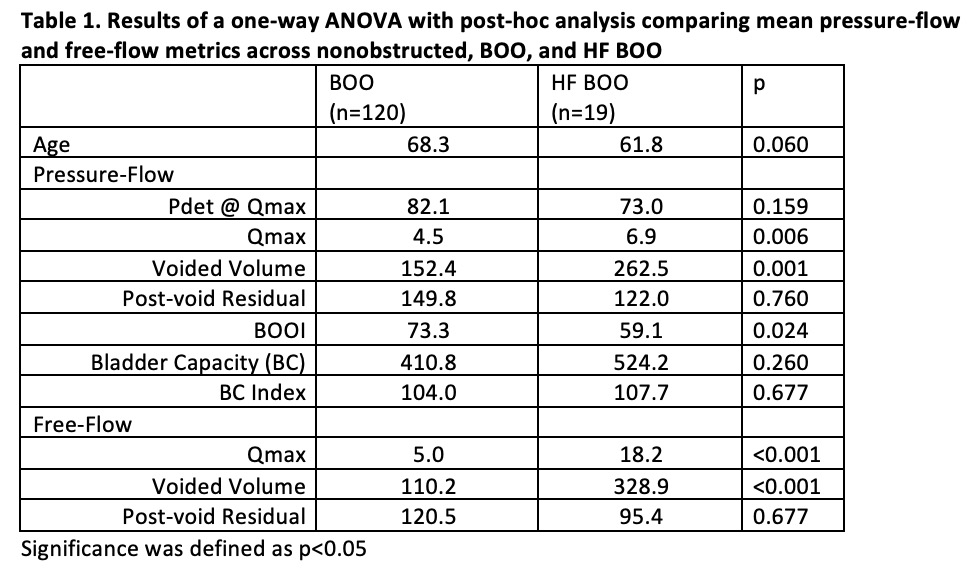
Results: Of 389 men with LUTS who underwent VUDS, 139 met criteria for BOO and 19 (13.7%) had HF BOO. Compared to men with BOO, HF BOO patients had significantly higher pressure-flow Qmax, voided volume, and free-flow Qmax and voided volume (Table 1). Conservatively managed patients (n=10) had a mean decrease in Qmax of 5.3 mL/s, as opposed to a mean increase in Qmax of 18.3 mL/s for those who elected surgical treatment (n=4) (p=0.241 and 0.167, respectively).
Conclusions: This data suggest that a normal uroflow does not rule out BOO. HF BOO was seen in 14% of men with VUDS proven BOO, consistent with two previous studies. This suggests that about 1 in 7 men may be misdiagnosed as non-obstructed based on screening free-flow uroflowmetry, which could lead to inappropriate management. We are encouraged by our observations of an increase in Qmax in the subset of HF BOO patients who underwent surgery, but the sample is too small to draw meaningful conclusions. The clinical implications of HF BOO have not been well described and warrant further evaluation to improve the diagnostic and treatment algorithm for BOO.
Source of Funding: None.
Methods: This was a retrospective review of an ongoing database of men with refractory lower urinary tract symptoms (LUTS) who underwent videourodynamic studies (VUDS). Patient demographics and urodynamics data were collected, and those with incomplete data or erroneous urodynamic tracings were excluded. Patients were diagnosed with BOO if the BOOI > 40 and HF BOO if a contemporaneous pressure or free-flow Qmax = 15 mL/s. A two-tailed independent sample t-test was conducted to compare urodynamic parameters between men with BOO and men with HF BOO. For HF BOO patients, post-treatment free-flow values were compared when treated conservatively and surgically.
Results: Of 389 men with LUTS who underwent VUDS, 139 met criteria for BOO and 19 (13.7%) had HF BOO. Compared to men with BOO, HF BOO patients had significantly higher pressure-flow Qmax, voided volume, and free-flow Qmax and voided volume (Table 1). Conservatively managed patients (n=10) had a mean decrease in Qmax of 5.3 mL/s, as opposed to a mean increase in Qmax of 18.3 mL/s for those who elected surgical treatment (n=4) (p=0.241 and 0.167, respectively).
Conclusions: This data suggest that a normal uroflow does not rule out BOO. HF BOO was seen in 14% of men with VUDS proven BOO, consistent with two previous studies. This suggests that about 1 in 7 men may be misdiagnosed as non-obstructed based on screening free-flow uroflowmetry, which could lead to inappropriate management. We are encouraged by our observations of an increase in Qmax in the subset of HF BOO patients who underwent surgery, but the sample is too small to draw meaningful conclusions. The clinical implications of HF BOO have not been well described and warrant further evaluation to improve the diagnostic and treatment algorithm for BOO.
Source of Funding: None.

.jpg)
.jpg)