Back
Poster, Podium & Video Sessions
Podium
PD39: Benign Prostatic Hyperplasia: Epidemiology, Evaluation & Medical Non-surgical Therapy
PD39-08: Implementation of a Simple Clinical Pathway Increases Relevance of Inpatient Consults for Urinary Retention
Sunday, May 15, 2022
8:10 AM – 8:20 AM
Location: Room 243
Luke Griffiths*, Darian Andreas, Shannon Smith, Aaron Smith, Hollie Brown, Jessica Kreshover, Justin Han, New Hyde Park, NY

Luke Griffiths, MD
Smith Institute for Urology, Zucker School of Medicine at Hofstra-Northwell
Podium Presenter(s)
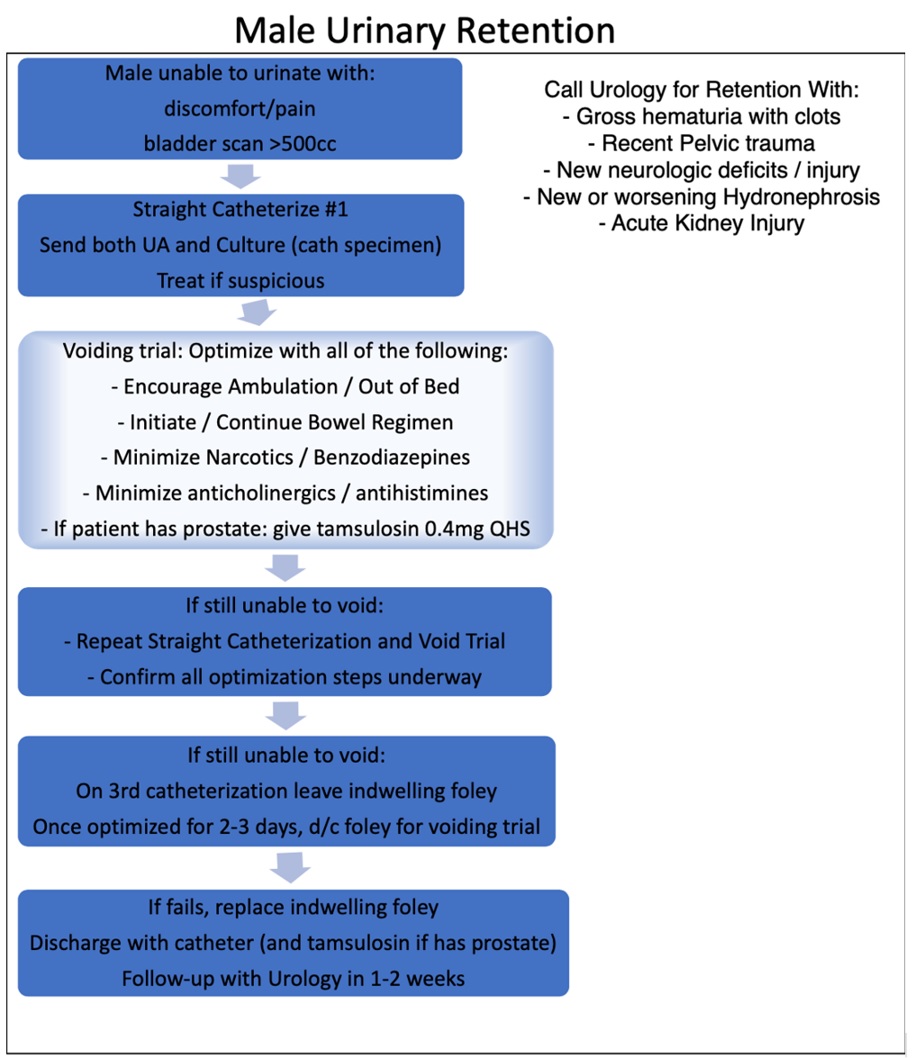
Introduction: Inpatient consultations are sometimes initiated in order to “establish care” without any acute need for specialist services. This creates additional expense for the health system while potentially delaying patient care and/or discharge. Urinary retention is often straightforward, requiring only bladder rest and medical optimization prior to trial of void in the outpatient setting for resolution. We sought to evaluate whether or not a simple decision tree could assist medical hospitalists in appropriately selecting patients requiring inpatient urologic management from those who can be safely directed to outpatient care.
Methods: Consults for urinary retention were identified based on billing data from July 2019 through June 2021. Male and female retention guideline policies were implemented to assist primary teams in determining if a patient’s retention could be managed via simple algorithm, or were deemed complex and requiring of inpatient urologic evaluation. Consults were considered complex if associated with gross hematuria with clots, recent pelvic trauma, neurologic deficits/injury, new or worsening hydronephrosis, or acute kidney injury. Patients were grouped into a pre-intervention 8-month period of July 2019 through February 2020, which was compared to a post intervention 10-month period of September 2020 through June 2021. March to August 2020 were excluded due to COVID-19 hospital volume changes. Chi square analysis was performed.
Results: A total of 163 retention consults were placed over the 18 study months. In the pre-intervention period, urology consultation was only truly required in 27/80 (33.8%). After implementation of the pathway, this significantly increased to 47/83 (56.6%,p = 0.003). Furthermore while the percentage of monthly consults requiring inpatient consultation increased in the post-intervention period, the overall total number of consults decreased from 10.0/month to 8.3/month.
Conclusions: Implementation of this urinary retention pathway increased the number of relevant inpatient consults while decreasing the number of simple retention consults. The net effect was a decrease in overall consults. This simple pathway may have identified more complex patients while reducing overutilization of specialist care.
Source of Funding: none
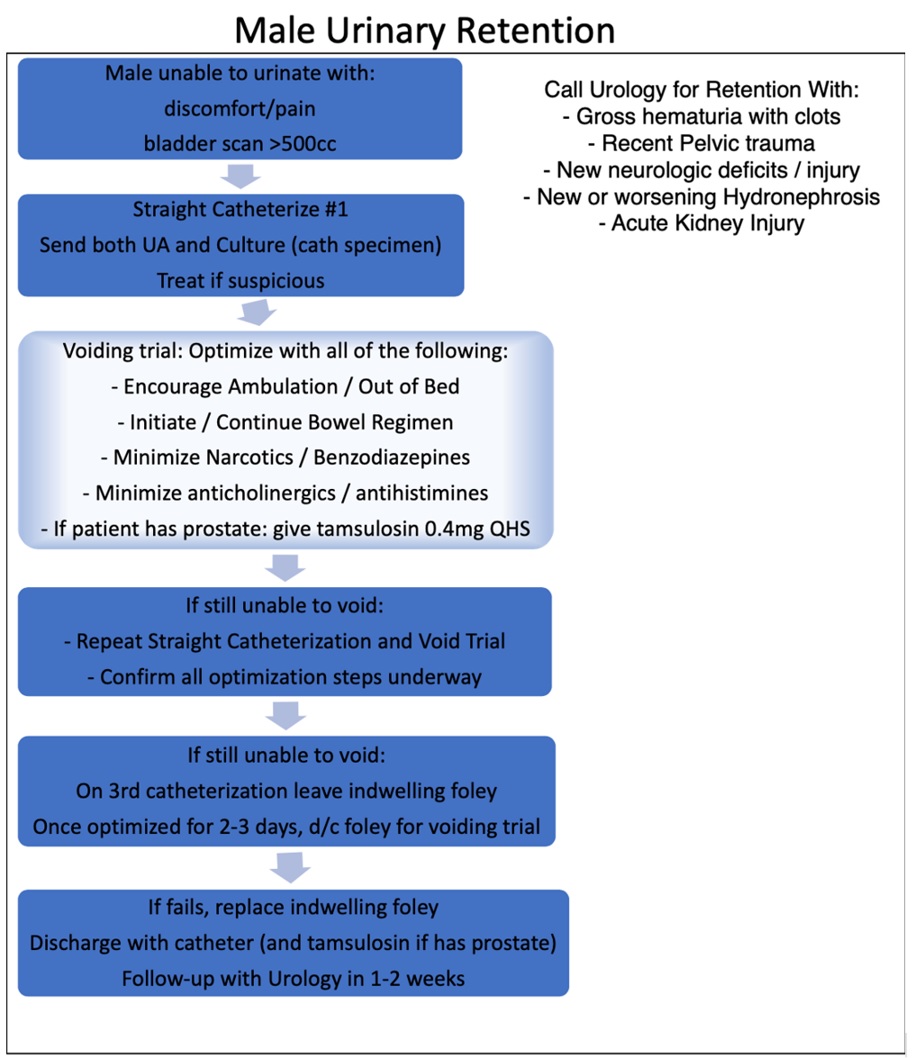
Methods: Consults for urinary retention were identified based on billing data from July 2019 through June 2021. Male and female retention guideline policies were implemented to assist primary teams in determining if a patient’s retention could be managed via simple algorithm, or were deemed complex and requiring of inpatient urologic evaluation. Consults were considered complex if associated with gross hematuria with clots, recent pelvic trauma, neurologic deficits/injury, new or worsening hydronephrosis, or acute kidney injury. Patients were grouped into a pre-intervention 8-month period of July 2019 through February 2020, which was compared to a post intervention 10-month period of September 2020 through June 2021. March to August 2020 were excluded due to COVID-19 hospital volume changes. Chi square analysis was performed.
Results: A total of 163 retention consults were placed over the 18 study months. In the pre-intervention period, urology consultation was only truly required in 27/80 (33.8%). After implementation of the pathway, this significantly increased to 47/83 (56.6%,p = 0.003). Furthermore while the percentage of monthly consults requiring inpatient consultation increased in the post-intervention period, the overall total number of consults decreased from 10.0/month to 8.3/month.
Conclusions: Implementation of this urinary retention pathway increased the number of relevant inpatient consults while decreasing the number of simple retention consults. The net effect was a decrease in overall consults. This simple pathway may have identified more complex patients while reducing overutilization of specialist care.
Source of Funding: none

.jpg)
.jpg)