Back
Poster, Podium & Video Sessions
Podium
PD41: Prostate Cancer: Detection & Screening IV
PD41-09: Moving Beyond PSA: Identifying the Optimal Diagnostic Strategy to Assess Prostate Cancer Risk
Sunday, May 15, 2022
10:50 AM – 11:00 AM
Location: Room 255
Douglas Cheung*, Diana Magee, Toronto, Canada, Thomas Stonier, London, United Kingdom, Andrew Briggs, Bart Ferket, New York, NY, Antonio Finelli, Girish Kulkarni, Toronto, Canada, Andrew Vickers, Sigrid Carlsson, James Eastham, New York, NY
- DC
Podium Presenter(s)
Introduction: Diagnostic strategies based on biomarkers and/or magnetic resonance imaging (MRI) may better select men whose PSA test is unlikely to be clinically significant prostate cancer (PCa) from men who may harbor life threatening disease. However, there is limited evidence regarding the combined use of biomarkers with MRI, and which sequence is most efficient. We compared the clinical- and cost-effectiveness of multiple strategies for the diagnosis of PCa.
Methods: A clinical decision tree was constructed (TreeAgePro 2021) to evaluate biomarker and MRI strategies versus systematic biopsy. In addition to solo testing, combination pathways of biomarkers and MRI with sequential testing in positive-reflexive (e.g. to locate the lesion) and negative-reflexive (e.g. to confirm the negative) manners were evaluated. Patients with a positive MRI and/or biomarker were biopsied. The base case was a biopsy-naïve man with a worrisome PSA for initial diagnosis. Our co-primary outcomes were: I) clinically significant (Gleason 3+4 or higher) and II) non-clinically significant PCa, III) biopsies avoided, and IV) mean cost (U.S. [$] and U.K. [£]) per patient. Model parameters were populated from a literature search of electronic databases (i.e. MEDLINE, PubMed). Inputs for diagnostic performance were preferentially identified using template biopsy reference standards. Cost data were selected from primary sources (e.g. governmental agencies) where available.
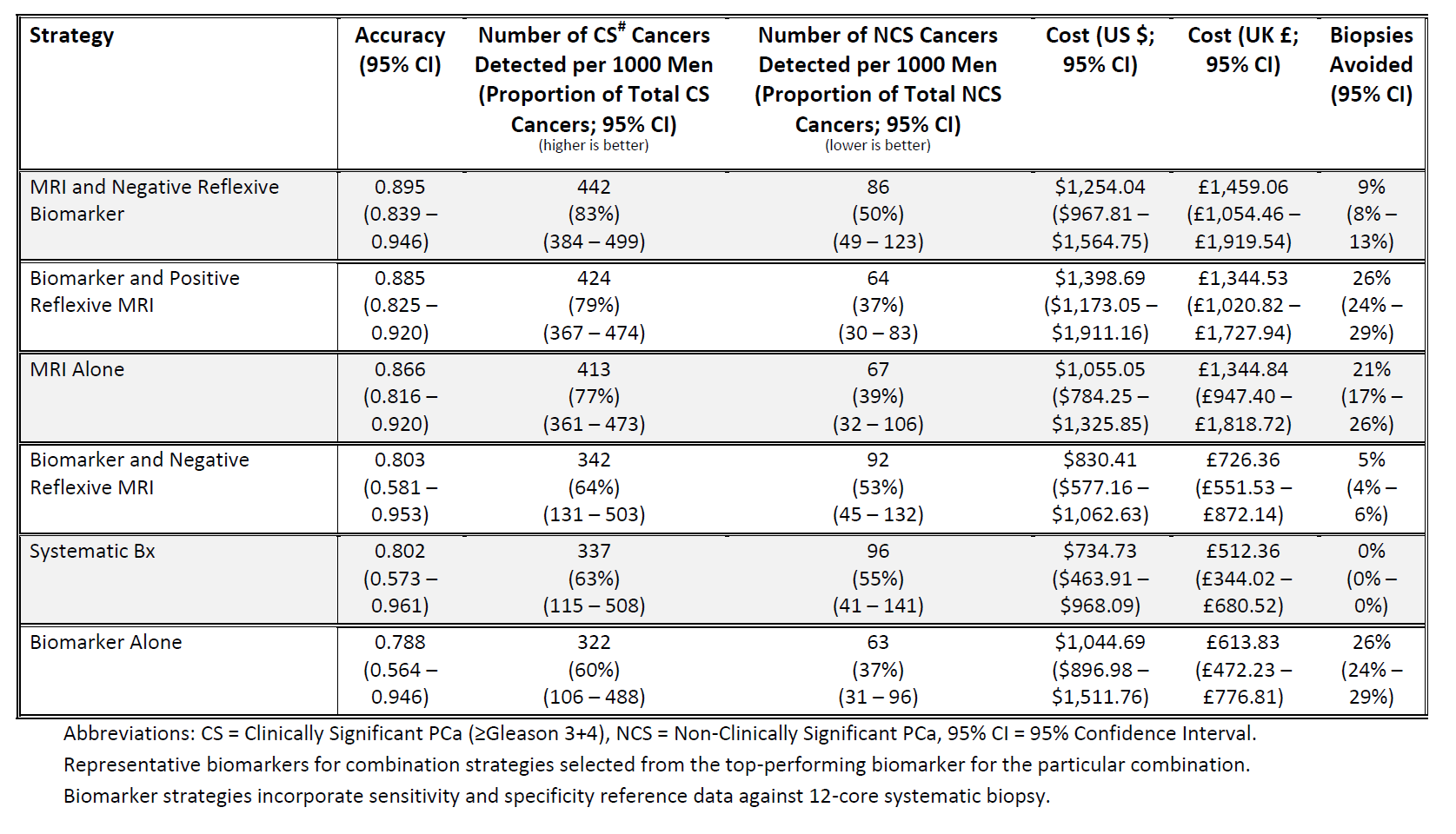
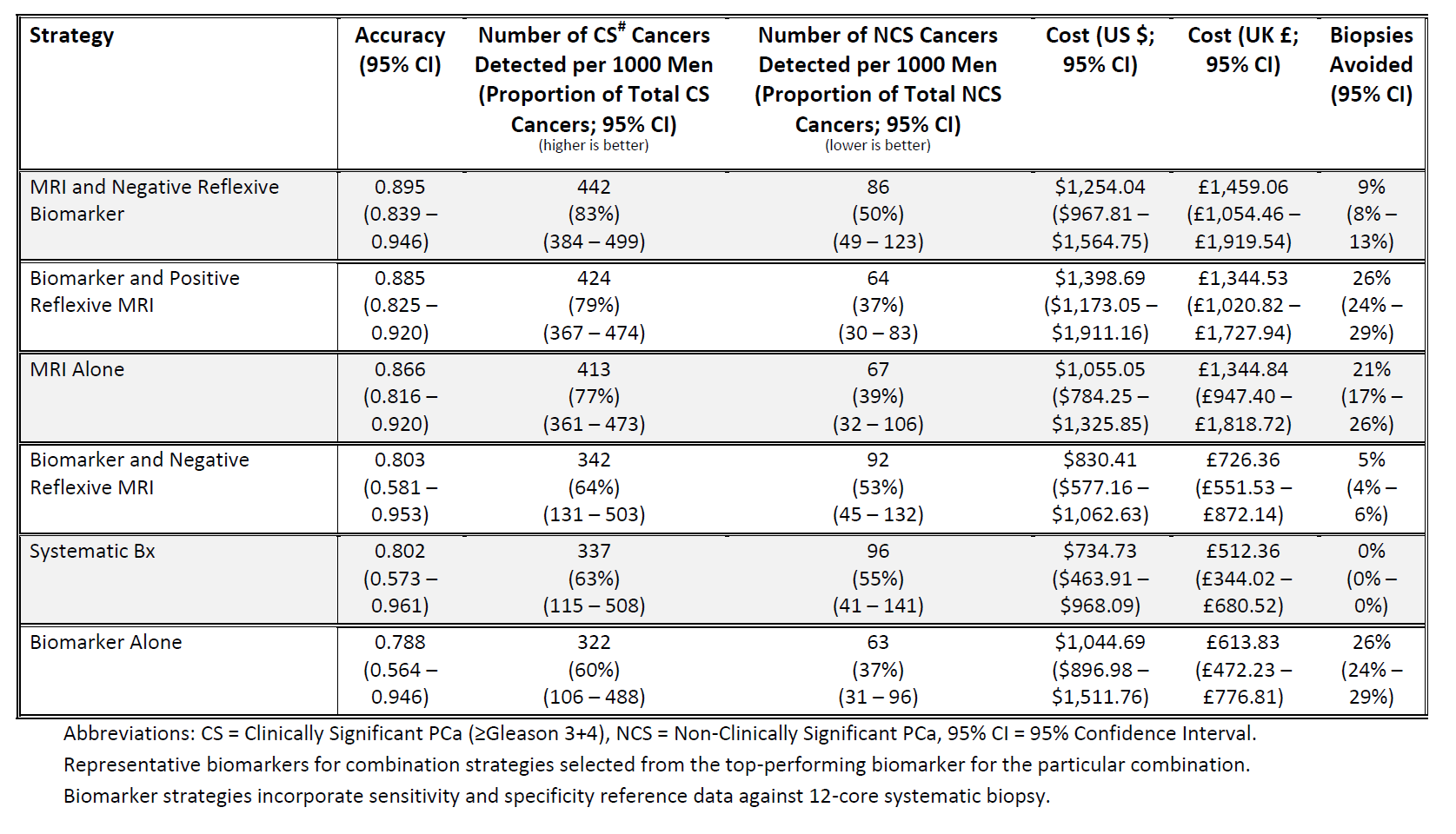
Results: Most combination strategies and MRI-alone were superior to a recommendation that all men with a worrisome PSA test undergo systematic biopsy (Table 1). Additional testing increased detection of clinically significant PCa (1%-19%), reduced overdiagnosing non-clinically significant PCa (2%-18%), while sparing many men from biopsy (5%-26%). There was a modest additional cost from $96-$933/£214-£1,161. Approaches that optimized clinical consequences and cost were biomarker with positive reflexive MRI or MRI followed by negative reflex biomarker. Our results were robust to sensitivity analyses exploring PCa prevalence and target-only biopsy.
Conclusions: Cost-effective pre-biopsy strategies including a combination of MRI and biomarker better identify men at higher risk for clinically significant PCa while avoiding biopsy in lower risk individuals.
Source of Funding: D.C.C.'s work was supported in part by the Canadian Institutes of Health Research Canada Graduate Doctoral Scholarship, Hold'em for Life Oncology Clinician Scientist/Fellowship, Canadian Association for Healthcare Reimbursement Research Scholarship, and Clinician Investigator Program-Ministry of Health Scholarship funding. A.B.’s, A.V.’s, S.V.C.’s and J.A.E.’s work was supported in part by funding from National Institutes of Health/National Cancer Institute (P30-CA008748) and Sidney Kimmel Center for Prostate and Urologic Cancers. S.V.C. was further supported by the National Institutes of Health/National Cancer Institute (K22-CA234400 and U01-CA199338-02) and the Prevent Cancer Foundation.
Methods: A clinical decision tree was constructed (TreeAgePro 2021) to evaluate biomarker and MRI strategies versus systematic biopsy. In addition to solo testing, combination pathways of biomarkers and MRI with sequential testing in positive-reflexive (e.g. to locate the lesion) and negative-reflexive (e.g. to confirm the negative) manners were evaluated. Patients with a positive MRI and/or biomarker were biopsied. The base case was a biopsy-naïve man with a worrisome PSA for initial diagnosis. Our co-primary outcomes were: I) clinically significant (Gleason 3+4 or higher) and II) non-clinically significant PCa, III) biopsies avoided, and IV) mean cost (U.S. [$] and U.K. [£]) per patient. Model parameters were populated from a literature search of electronic databases (i.e. MEDLINE, PubMed). Inputs for diagnostic performance were preferentially identified using template biopsy reference standards. Cost data were selected from primary sources (e.g. governmental agencies) where available.
Results: Most combination strategies and MRI-alone were superior to a recommendation that all men with a worrisome PSA test undergo systematic biopsy (Table 1). Additional testing increased detection of clinically significant PCa (1%-19%), reduced overdiagnosing non-clinically significant PCa (2%-18%), while sparing many men from biopsy (5%-26%). There was a modest additional cost from $96-$933/£214-£1,161. Approaches that optimized clinical consequences and cost were biomarker with positive reflexive MRI or MRI followed by negative reflex biomarker. Our results were robust to sensitivity analyses exploring PCa prevalence and target-only biopsy.
Conclusions: Cost-effective pre-biopsy strategies including a combination of MRI and biomarker better identify men at higher risk for clinically significant PCa while avoiding biopsy in lower risk individuals.
Source of Funding: D.C.C.'s work was supported in part by the Canadian Institutes of Health Research Canada Graduate Doctoral Scholarship, Hold'em for Life Oncology Clinician Scientist/Fellowship, Canadian Association for Healthcare Reimbursement Research Scholarship, and Clinician Investigator Program-Ministry of Health Scholarship funding. A.B.’s, A.V.’s, S.V.C.’s and J.A.E.’s work was supported in part by funding from National Institutes of Health/National Cancer Institute (P30-CA008748) and Sidney Kimmel Center for Prostate and Urologic Cancers. S.V.C. was further supported by the National Institutes of Health/National Cancer Institute (K22-CA234400 and U01-CA199338-02) and the Prevent Cancer Foundation.

.jpg)
.jpg)