Back
Poster, Podium & Video Sessions
Podium
PD47: Sexual Function/Dysfunction: Evaluation II
PD47-07: Rate of Prior Invasive Pelvic Procedures, Co-Diagnoses, and Treatment Choices in Women Presenting with Dyspareunia - A United States Claims Database Analysis
Sunday, May 15, 2022
2:00 PM – 2:10 PM
Location: Room 245
Kathryn Dumas, Baltimore, MD, Corey Able, Galveston, TX, Jaden R Kohn, Taylor P Kohn*, Marisa Clifton, Baltimore, MD
- TK
Taylor Kohn, MD
MD, MPhil
Podium Presenter(s)
Introduction: The International Continence Society defines dyspareunia as “persistent or recurrent pain or discomfort associated with attempted or complete vaginal penetration.” As the incidence of dyspareunia depends on the definition used and the population studied, dyspareunia is inadequately characterized in the current literature. The objective of this study was to identify baseline characteristics and subsequent treatments for women receiving a diagnosis of dyspareunia utilizing a large US claims database.
Methods: The TriNetX Diamond network database was queried - a US health research network consisting of 190 million patients and encompassing health care encounters between 2009-2021. Incidence of dyspareunia (ICD10 N94.1) in women over the age of 18 was calculated for 2009-2012, 2013-2016, and 2017-2021. Co-morbidities and pelvic procedures were identified prior to the date of dyspareunia diagnosis. Subsequent therapies were identified within 60 days after the initial diagnosis of dyspareunia.
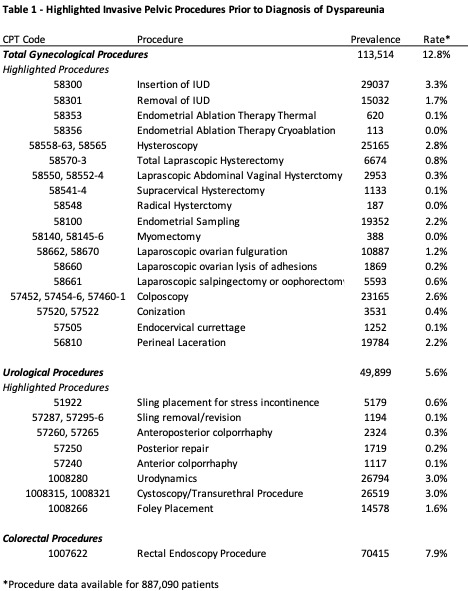
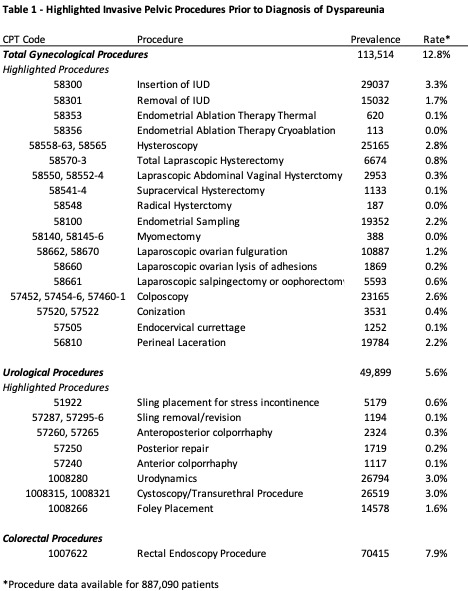
Results: A total of 1,089,728 unique patients had a diagnosis of dyspareunia with an average age of 41.3±14.8 years. There was a high rate of reported prior invasive pelvic procedures at 30.7% (Table 1). Women also had high rates of co-diagnoses of chronic back pain (48.4%), anxiety (37.1%), sleep disorders (21.7%), migraines (18.4%), vascular headaches (18.1%), and constipation (18.9%).
In the initial 60 days after initial diagnosis of dyspareunia, only 766 women (0.07%) were prescribed pelvic floor therapy (CPT 90901 or 90911). Only 6.8% were prescribed vaginal estrogen (4.5% of women with dyspareunia age 18-54 and 15.1% of women with dyspareunia age >54), while 1.7% were prescribed gabapentin, 0.8% venlafaxine, and 0.5% ospemifene. Notably, 9.7% were prescribed opioids and 5.1% were prescribed benzodiazepines with 3.9% receiving both an opioid prescription and benzodiazepine prescription within 60 days of index diagnosis of dyspareunia.
Conclusions: Dyspareunia is an increasingly identified diagnosis and often associated with prior invasive pelvic procedures. Rates of prescribing vaginal estrogen and pelvic floor therapy are low while prescribing of benzodiazepines and opioids initially after diagnosis are relatively elevated.
Source of Funding: None
Methods: The TriNetX Diamond network database was queried - a US health research network consisting of 190 million patients and encompassing health care encounters between 2009-2021. Incidence of dyspareunia (ICD10 N94.1) in women over the age of 18 was calculated for 2009-2012, 2013-2016, and 2017-2021. Co-morbidities and pelvic procedures were identified prior to the date of dyspareunia diagnosis. Subsequent therapies were identified within 60 days after the initial diagnosis of dyspareunia.
Results: A total of 1,089,728 unique patients had a diagnosis of dyspareunia with an average age of 41.3±14.8 years. There was a high rate of reported prior invasive pelvic procedures at 30.7% (Table 1). Women also had high rates of co-diagnoses of chronic back pain (48.4%), anxiety (37.1%), sleep disorders (21.7%), migraines (18.4%), vascular headaches (18.1%), and constipation (18.9%).
In the initial 60 days after initial diagnosis of dyspareunia, only 766 women (0.07%) were prescribed pelvic floor therapy (CPT 90901 or 90911). Only 6.8% were prescribed vaginal estrogen (4.5% of women with dyspareunia age 18-54 and 15.1% of women with dyspareunia age >54), while 1.7% were prescribed gabapentin, 0.8% venlafaxine, and 0.5% ospemifene. Notably, 9.7% were prescribed opioids and 5.1% were prescribed benzodiazepines with 3.9% receiving both an opioid prescription and benzodiazepine prescription within 60 days of index diagnosis of dyspareunia.
Conclusions: Dyspareunia is an increasingly identified diagnosis and often associated with prior invasive pelvic procedures. Rates of prescribing vaginal estrogen and pelvic floor therapy are low while prescribing of benzodiazepines and opioids initially after diagnosis are relatively elevated.
Source of Funding: None

.jpg)
.jpg)