Back
Poster, Podium & Video Sessions
Podium
PD54: Prostate Cancer: Localized: Surgical Therapy III
PD54-05: Halsteadian View of Prostate Cancer: Does removing more nodes at radical prostatectomy affect biochemical recurrence?
Monday, May 16, 2022
7:40 AM – 7:50 AM
Location: Room 245
Lior Taich*, Los Angeles, CA, Lin Gu, Durham, NC, Christopher L. Amling, Portland, OR, William J. Aronson, Los Angeles, CA, Matthew R. Cooperberg, San Francisco, CA, Lourdes G. Rivera, San Juan, Puerto Rico, Christopher J. Kane, San Diego, CA, Zachary Klassen, Martha K. Terris, augusta, GA, Stephen Freedland, Los Angeles, CA
- LT
Podium Presenter(s)
Introduction: The extent of lymph node dissection during radical prostatectomy (RP) is a long debated issue. Most recently in prostate cancer, standard vs. extended lymph node dissection was evaluated in a randomized control trial, yet the both groups had a high number of nodes removed and varied by only 2 nodes (12 vs. 14). We evaluated whether more nodes taken at RP was associated with better outcomes in a Veteran Affairs (VA) population.
Methods: The shared equal access regional cancer hospital (SEARCH) database was queried for patients diagnosed with prostate cancer who underwent RP between 2000-2020. Patients were excluded if they underwent neoadjuvant therapy, did not have lymph nodes removed at time of surgery, or did not have PSA data after surgery. Number of lymph nodes removed was treated as a continuous variable. Hazard Ratios (HRs) and 95% confidence intervals (CIs) of biochemical recurrence (BCR), overall survival (OS), metastasis, castrate resistant prostate cancer (CRPC), and prostate cancer specific mortality (PCSM) were estimated using Cox proportional hazard method adjusting for age, race, surgical year, Charlson comorbidity index (CCI), biopsy Gleason score, and log-transformed PSA.
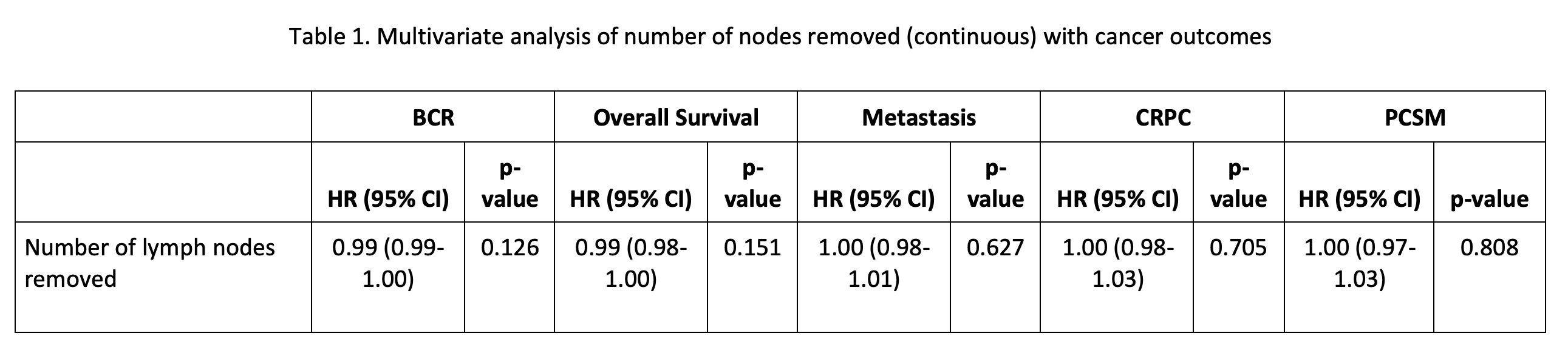
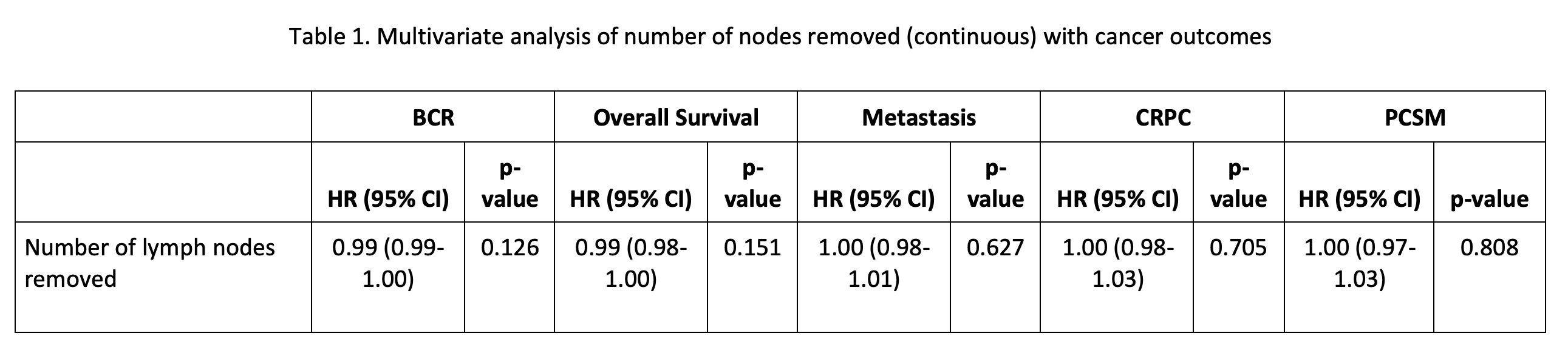
Results: 4,255 patients were included in the analysis. The average age was 63 and average PSA was 9.5. White men comprised 70% of the dataset, Black men represented 26%, and 4% were Other. There were 9 lymph nodes removed on average, with biopsy Gleason <6 having 7 removed, Gleason 3+4 and 4+3 had 9 removed, and 11 nodes were removed in Gleason 8-10 (p < 0.001). The number of lymph nodes removed did not have a statistically significant impact on BCR (HR 0.99, 95% CI 0.99-1.00, p=0.126), or on OS, metastasis, CRPC, or PCSM.
Conclusions: The extent of lymph node dissection during RP seen in the SEARCH cohort is in line with prior literature, and predictably, patients with more aggressive disease had more nodes removed. In our real world dataset, removing more lymph nodes at RP did not improve BCR or survival. These data suggest that an extended lymph node dissection may provide more diagnostic utility than therapeutic benefit.
Source of Funding: None
Methods: The shared equal access regional cancer hospital (SEARCH) database was queried for patients diagnosed with prostate cancer who underwent RP between 2000-2020. Patients were excluded if they underwent neoadjuvant therapy, did not have lymph nodes removed at time of surgery, or did not have PSA data after surgery. Number of lymph nodes removed was treated as a continuous variable. Hazard Ratios (HRs) and 95% confidence intervals (CIs) of biochemical recurrence (BCR), overall survival (OS), metastasis, castrate resistant prostate cancer (CRPC), and prostate cancer specific mortality (PCSM) were estimated using Cox proportional hazard method adjusting for age, race, surgical year, Charlson comorbidity index (CCI), biopsy Gleason score, and log-transformed PSA.
Results: 4,255 patients were included in the analysis. The average age was 63 and average PSA was 9.5. White men comprised 70% of the dataset, Black men represented 26%, and 4% were Other. There were 9 lymph nodes removed on average, with biopsy Gleason <6 having 7 removed, Gleason 3+4 and 4+3 had 9 removed, and 11 nodes were removed in Gleason 8-10 (p < 0.001). The number of lymph nodes removed did not have a statistically significant impact on BCR (HR 0.99, 95% CI 0.99-1.00, p=0.126), or on OS, metastasis, CRPC, or PCSM.
Conclusions: The extent of lymph node dissection during RP seen in the SEARCH cohort is in line with prior literature, and predictably, patients with more aggressive disease had more nodes removed. In our real world dataset, removing more lymph nodes at RP did not improve BCR or survival. These data suggest that an extended lymph node dissection may provide more diagnostic utility than therapeutic benefit.
Source of Funding: None

.jpg)
.jpg)