Back
Poster, Podium & Video Sessions
Podium
PD56: Kidney Cancer: Localized: Surgical Therapy IV
PD56-01: Improved Prediction of Renal Function after Radical Nephrectomy
Monday, May 16, 2022
9:30 AM – 9:40 AM
Location: Room 255
Nityam Rathi*, Yosuke Yasuda, Diego Aguilar Palacios, Cleveland, OH, Yunlin Ye, Guangzhou, China, People's Republic of, Jianbo Li, Christopher Weight, Mohammed Eltemamy, Robert Abouassaly, Steven Campbell, Cleveland, OH
- NR
Podium Presenter(s)
Introduction: Radical nephrectomy (RN) is an important consideration for the surgical management of localized renal cell carcinoma (RCC), particularly in cases of increased oncologic potential. However, reduced renal function after RN is a concern. Preoperative global glomerular filtration rate (GFR) and split renal function (SRF) in the contralateral kidney have been shown to be strong predictors of new baseline GFR (NBGFR) post-RN. Recently, software has been developed to perform parenchymal volume analysis (PVA) on preoperative imaging to determine SRF (FUJIFILM Medical Systems). We compare the abilities of two SRF-based models, using either nuclear renal scan (NRS) or PVA to determine SRF, to predict NBGFR after RN. These SRF-based models were also compared with subjective prediction of NBGFR by an experienced urologic oncologist, because some believe that an expert can predict such outcomes accurately and that predictive models may not be needed in this domain.
Methods: All 187 RCC patients who underwent RN (2006-16) with preoperative CT/MRI, NRS, and preop/postoperative GFR estimations were analyzed. NBGFR was defined as GFR 3-12 months after RN. For the two SRF-based approaches, SRF was derived from either NRS or semi-automated PVA software, and renal functional compensation was estimated at 25% based on previous studies. Thus, the formula (Global GFRPre-RN × SRFcontralateral) x 1.25 was used to predict NBGFR. For the “Subjective Approach”, a blinded, independent urologic oncologist provided predictions of NBGFR based on preoperative CT/MRI, baseline global GFR, tumor features, and patient age/comorbidities. Predictive accuracies were assessed by correlation coefficients (r).
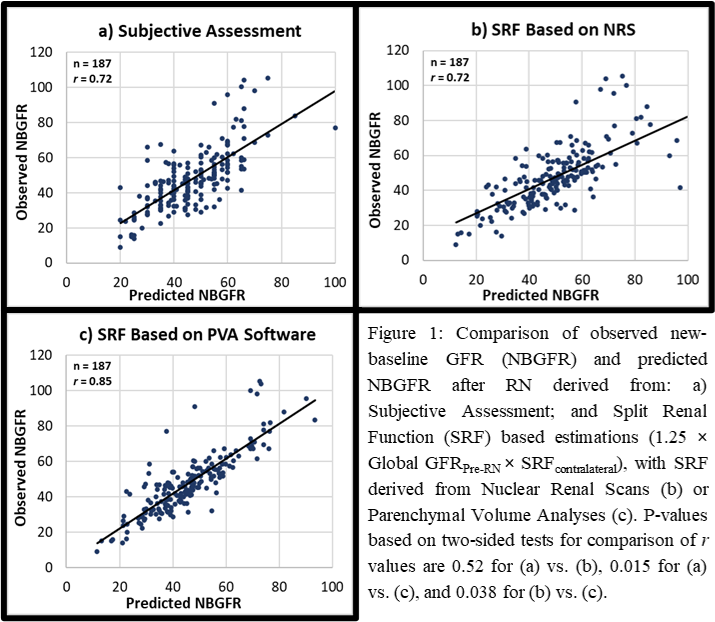
Results: The r for the Subjective Assessment, NRS/SRF-based, and PVA/SRF-based approaches were 0.72, 0.72, and 0.85, respectively (Fig. 1). An SRF-based model using PVA to determine SRF performed better than NRS/SRF-based and Subjective approaches (both p < 0.05).
Conclusions: Software-based PVA more accurately predicts NBGFR after RN than NRS and Subjective Assessment. The readily-available, inexpensive PVA software provides a precise and accurate estimation of SRF from routine preoperative CT/MRI. Clinically, this practical and innovative approach can contribute to the assessment of the merits and risks of RN versus partial nephrectomy in complex RCC cases.
Source of Funding: None
Methods: All 187 RCC patients who underwent RN (2006-16) with preoperative CT/MRI, NRS, and preop/postoperative GFR estimations were analyzed. NBGFR was defined as GFR 3-12 months after RN. For the two SRF-based approaches, SRF was derived from either NRS or semi-automated PVA software, and renal functional compensation was estimated at 25% based on previous studies. Thus, the formula (Global GFRPre-RN × SRFcontralateral) x 1.25 was used to predict NBGFR. For the “Subjective Approach”, a blinded, independent urologic oncologist provided predictions of NBGFR based on preoperative CT/MRI, baseline global GFR, tumor features, and patient age/comorbidities. Predictive accuracies were assessed by correlation coefficients (r).
Results: The r for the Subjective Assessment, NRS/SRF-based, and PVA/SRF-based approaches were 0.72, 0.72, and 0.85, respectively (Fig. 1). An SRF-based model using PVA to determine SRF performed better than NRS/SRF-based and Subjective approaches (both p < 0.05).
Conclusions: Software-based PVA more accurately predicts NBGFR after RN than NRS and Subjective Assessment. The readily-available, inexpensive PVA software provides a precise and accurate estimation of SRF from routine preoperative CT/MRI. Clinically, this practical and innovative approach can contribute to the assessment of the merits and risks of RN versus partial nephrectomy in complex RCC cases.
Source of Funding: None

.jpg)
.jpg)