Back
Poster, Podium & Video Sessions
Podium
PD59: Kidney Cancer: Advanced (including Drug Therapy) II
PD59-07: Neglected lymph nodal metastases in patients with renal cancer: when to extend the anatomical template of lymph node dissection during nephrectomy
Monday, May 16, 2022
2:00 PM – 2:10 PM
Location: Room 255
Giuseppe Rosiello*, Giuseppe Fallara, Giuseppe Basile, Daniele Cignoli, Alberto Martini, Francesco De Cobelli, Giorgio Brembilla, Luigi Nocera, Federico Belladelli, Gianmarco Colandrea, Daniela Canibus, Chiara Re, Giacomo Musso, Francesco Cei, Rayan Matloob, Alberto Briganti, Roberto Bertini, Andrea Necchi, Daniele Raggi, Milan, Italy, Pierre I. Karakiewicz, Montreal, Canada, Francesco Montorsi, Andrea Salonia, Alessandro Larcher, Umberto Capitanio, Milan, Italy

Giuseppe Rosiello, MD
Resident
San Raffaele Hospital
Podium Presenter(s)
Introduction: The role of lymph node dissection (LND) in patients with renal cell carcinoma (RCC) is still controversial. For the first time, we tested the hypothesis that occulted lymph node invasion can be predicted according to the presence and the characteristics of lymphadenopathies at preoperative imaging.
Methods: Within a prospectively maintained database, we identified 797 patients with RCC and treated with partial or radical nephrectomy with or without LND at a single tertiary centre between 2000 and 2021. Lymphadenopathy (cN1) was defined as a suspicious lymph node with axial size >1 cm. Anatomical location of cN1 was categorized as follows: 1) hilar; 2) interaortocaval; 3) paraortic; 4) retrocaval. Extended LND (eLND) was defined as LND performed also outside the cN1 anatomical area. Multivariable logistic regression analyses tested for predictors of lymph node invasion (pN1) outside the anatomical field at imaging. A local polynomial smoother weighted function was used to graphically depict the effect of clinical lymph node size on the probability of pN1 outside the suspicious anatomical field, after accounting for tumor size and number of lymph node removed.
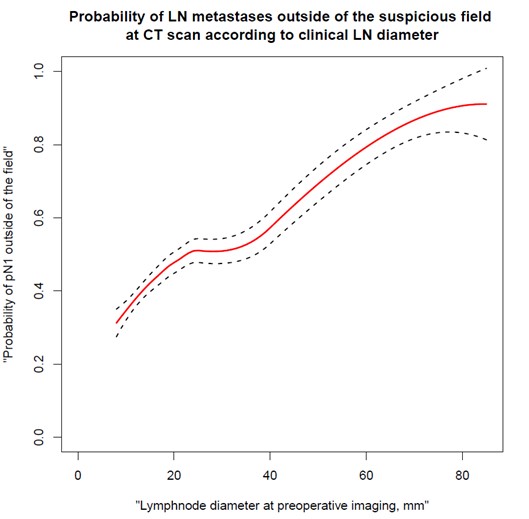
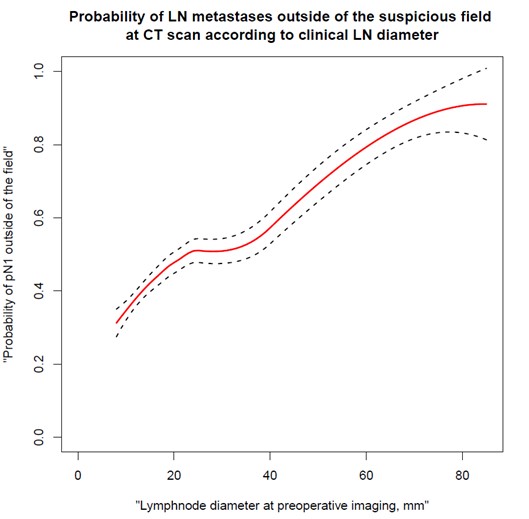
Results: Overall, 283 (35%) patients underwent LND. Median clinical tumor size was 5 (IQR: 3-7) cm. Proportion of pN1 was 46% vs. 4% in cN1 vs cN0 patients (p < 0.001). LND was extended outside cN1 anatomical location in 43% of the cases. Of these, 11% were pN0 and 3.2% vs. 22% vs. 6.4% had pN1 only inside vs. in and outside vs. only outside the suspicious area at preoperative imaging (p < 0.001), respectively. At multivariable analyses, lymph node size at imaging independently predicted the risk of lymph node invasion outside the suspicious area (Odds ratio: 1.05, 95%CI 1.02-.1.11; p=0.02 - Figure 1).
Conclusions: Approximately, one out of ten patients surgically treated for kidney cancer harbour suspicious LNI at preoperative imaging (cN1). In those cases, roughly 30% of the patients have occult lymph node metastases outside the anatomical area of cN1, as well. Lymph node size independently predict the risk of finding occult lymph node metastases outside the anatomical area cN1, indicating the need for a more extended LND in case of larger lymphadenopathies.
Source of Funding: no
Methods: Within a prospectively maintained database, we identified 797 patients with RCC and treated with partial or radical nephrectomy with or without LND at a single tertiary centre between 2000 and 2021. Lymphadenopathy (cN1) was defined as a suspicious lymph node with axial size >1 cm. Anatomical location of cN1 was categorized as follows: 1) hilar; 2) interaortocaval; 3) paraortic; 4) retrocaval. Extended LND (eLND) was defined as LND performed also outside the cN1 anatomical area. Multivariable logistic regression analyses tested for predictors of lymph node invasion (pN1) outside the anatomical field at imaging. A local polynomial smoother weighted function was used to graphically depict the effect of clinical lymph node size on the probability of pN1 outside the suspicious anatomical field, after accounting for tumor size and number of lymph node removed.
Results: Overall, 283 (35%) patients underwent LND. Median clinical tumor size was 5 (IQR: 3-7) cm. Proportion of pN1 was 46% vs. 4% in cN1 vs cN0 patients (p < 0.001). LND was extended outside cN1 anatomical location in 43% of the cases. Of these, 11% were pN0 and 3.2% vs. 22% vs. 6.4% had pN1 only inside vs. in and outside vs. only outside the suspicious area at preoperative imaging (p < 0.001), respectively. At multivariable analyses, lymph node size at imaging independently predicted the risk of lymph node invasion outside the suspicious area (Odds ratio: 1.05, 95%CI 1.02-.1.11; p=0.02 - Figure 1).
Conclusions: Approximately, one out of ten patients surgically treated for kidney cancer harbour suspicious LNI at preoperative imaging (cN1). In those cases, roughly 30% of the patients have occult lymph node metastases outside the anatomical area of cN1, as well. Lymph node size independently predict the risk of finding occult lymph node metastases outside the anatomical area cN1, indicating the need for a more extended LND in case of larger lymphadenopathies.
Source of Funding: no

.jpg)
.jpg)