Back
Poster, Podium & Video Sessions
Podium
PD60: Prostate Cancer: Localized: Surgical Therapy V
PD60-01: The impact of baseline health-related quality of life on biochemical recurrence free survival in high-risk prostate cancer patients following radical prostatectomy
Monday, May 16, 2022
1:00 PM – 1:10 PM
Location: Room 245
Thilo Westhofen*, Alexander Buchner, Boris Schlenker, Armin Becker, Christian G. Stief, Alexander Kretschmer, Munich, Germany
- TW
Podium Presenter(s)
Introduction: Several studies have shown baseline health-related quality of life (HRQOL) to be a valuable prognostic indicator of survival outcomes for various cancer entities in the metastatic setting. To date, there is no evidence regarding the prognostic value of baseline HRQOL for patients undergoing radical prostatectomy (RP) due to localized prostate cancer (PC). The objective of this study was to assess the impact of baseline preoperative HRQOL on survival prognosis for high-risk PC patients following RP.
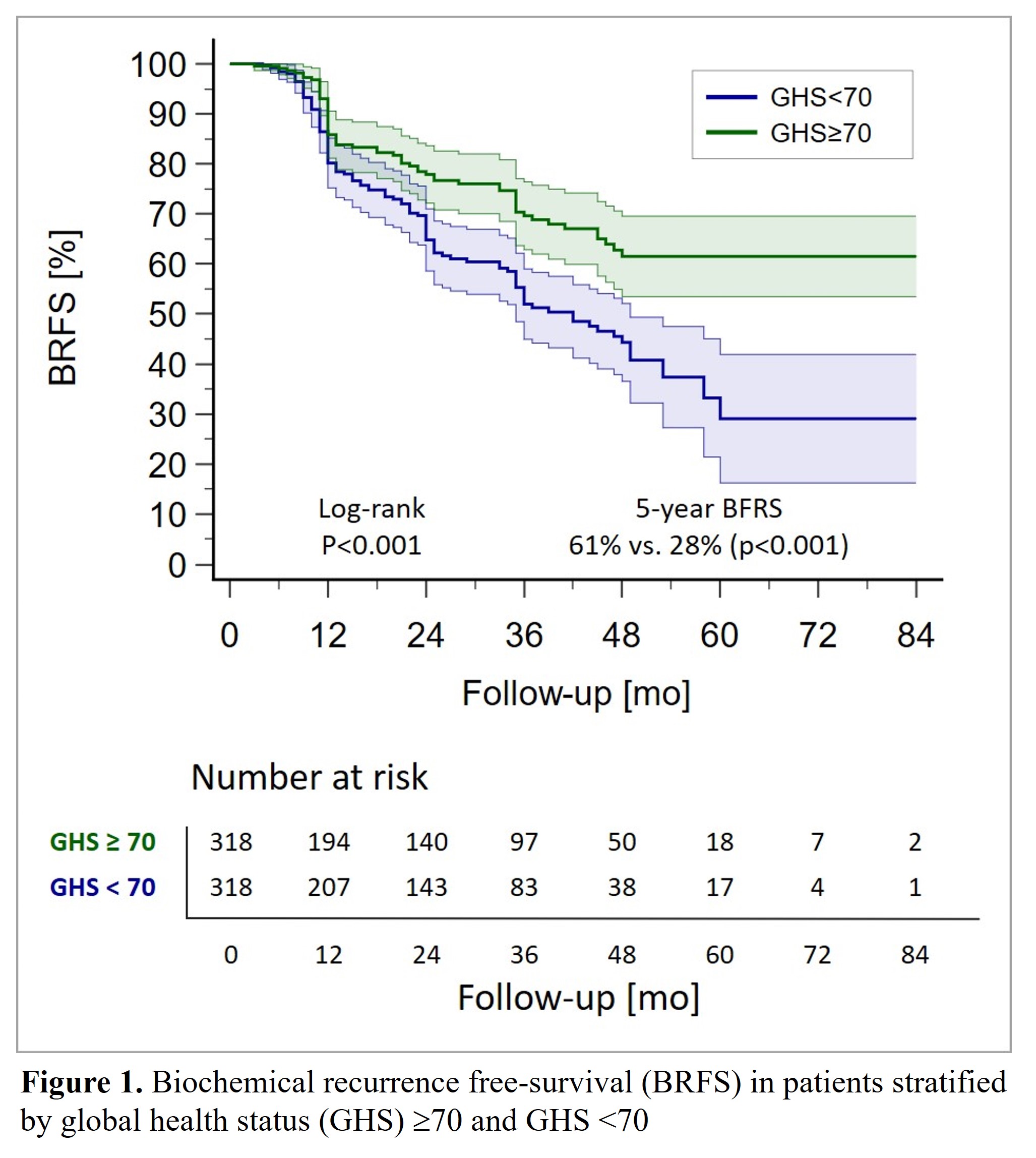
Methods: 1029 patients with high-risk PC according to NCCN risk stratification and prospectively assessed baseline HRQOL prior RP were included. Patients were stratified by the global health status (GHS) domain of the EORTC QLQ-C30 questionnaire, good general HRQOL was defined as GHS=70 based on validated cut-off levels. Subsequently, a propensity score-matched analysis of 636 patients [n=318 (GHS=70), n=318 (GHS <70)] was conducted. Primary endpoint was biochemical recurrence-free survival (BRFS), secondary endpoint was metastasis-free survival (MFS). Multivariate Cox regression models were performed to assess prognostic significance of baseline GHS on survival outcomes. Harrell’s discrimination C-index was applied to calculate the predictive accuracy of the model (p < 0.05).
Results: Median follow-up was 40mo. Applying matching variables age, PSA, pT stage, Gleason grade, positive surgical margin rate, and lymph node involvement, patients subcohorts were well-balanced. 5-yr-BRFS (61% vs. 28%; p<0.001) and 5-yr-MFS (86% vs. 68%; p=0.003) were significantly increased in the GHS=70 cohort. In multivariate analysis GHS=70 was confirmed as an independent predictor for increased BRFS (HR 0.60, 95%CI 0.44–0.82; p=0.013) and MFS (HR 0.51, 95%CI 0.30–0.87; p=0.026). Adding baseline HRQOL to our model improved predictive accuracy of BRFS by 8% (Harrell’s C-index of 0.69 vs 0.65).
Conclusions: Our findings highlight baseline HRQOL to be a valuable and robust prognostic factor for patients with localized high-risk PC prior RP. Baseline good general HRQOL accurately predicts increased BRFS and MFS.
Source of Funding: none
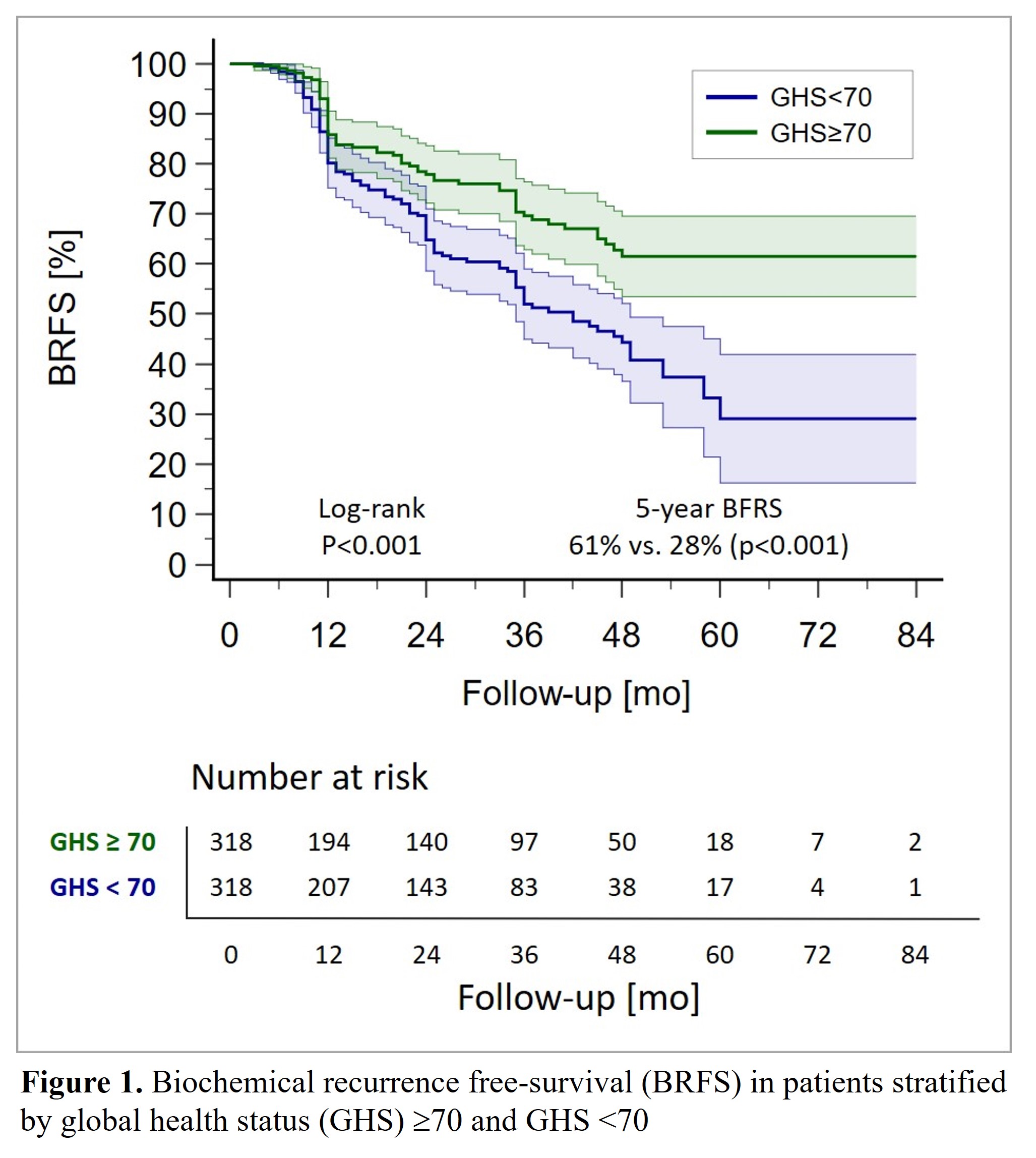
Methods: 1029 patients with high-risk PC according to NCCN risk stratification and prospectively assessed baseline HRQOL prior RP were included. Patients were stratified by the global health status (GHS) domain of the EORTC QLQ-C30 questionnaire, good general HRQOL was defined as GHS=70 based on validated cut-off levels. Subsequently, a propensity score-matched analysis of 636 patients [n=318 (GHS=70), n=318 (GHS <70)] was conducted. Primary endpoint was biochemical recurrence-free survival (BRFS), secondary endpoint was metastasis-free survival (MFS). Multivariate Cox regression models were performed to assess prognostic significance of baseline GHS on survival outcomes. Harrell’s discrimination C-index was applied to calculate the predictive accuracy of the model (p < 0.05).
Results: Median follow-up was 40mo. Applying matching variables age, PSA, pT stage, Gleason grade, positive surgical margin rate, and lymph node involvement, patients subcohorts were well-balanced. 5-yr-BRFS (61% vs. 28%; p<0.001) and 5-yr-MFS (86% vs. 68%; p=0.003) were significantly increased in the GHS=70 cohort. In multivariate analysis GHS=70 was confirmed as an independent predictor for increased BRFS (HR 0.60, 95%CI 0.44–0.82; p=0.013) and MFS (HR 0.51, 95%CI 0.30–0.87; p=0.026). Adding baseline HRQOL to our model improved predictive accuracy of BRFS by 8% (Harrell’s C-index of 0.69 vs 0.65).
Conclusions: Our findings highlight baseline HRQOL to be a valuable and robust prognostic factor for patients with localized high-risk PC prior RP. Baseline good general HRQOL accurately predicts increased BRFS and MFS.
Source of Funding: none

.jpg)
.jpg)