Back
Poster, Podium & Video Sessions
Moderated Poster
MP15: Prostate Cancer: Localized: Surgical Therapy I
MP15-19: Can low risk disease outside the Index lesion be left untreated in men suitable for focal therapy? Development of Novel criteria to identify potential candidates for focal therapy among patients with intermediate risk prostate cancer and positive multi-parametric MRI.
Friday, May 13, 2022
2:45 PM – 4:00 PM
Location: Room 222
Armando Stabile*, Giorgio Gandaglia, Elio Mazzone, Francesco Barletta, Daniele Robesti, Giuseppe Cirulli, Donato Cannoletta, Francesco Pellegrino, Luigi Nocera, Gabriele Sorce, Milan, Italy, Thomas Seisen, Morgan Roupret, Paris, France - Metropolitan, Jeffrey R. Karnes, Rochester, MN, Vito Cucchiara, Giuseppe Rosiello, Milan, Italy, Nicola Fossati, Lugano, Switzerland, Nazareno Suardi, Genoa, Italy, Francesco De Cobelli, Antonio Esposito, Giorgio Brembilla, Milan, Italy, Shahrokh Shariat, Vienna, Austria, Francesco Montorsi, Alberto Briganti, Milan, Italy

Armando Stabile, MD
Vita-Salute San Raffaele University
Poster Presenter(s)
Introduction: There is a lack of standardization to identify the optimal candidate for focal therapy (FT) among prostate cancer (PCa) patients. Moreover, whether low-risk disease outside IL can be left untreated is still unknown. We aimed at providing novel selection criteria among patients with intermediate-risk PCa and a suspicious visible lesion at MRI relying on men receiving radical prostatectomy (RP).
Methods: We relied on 173 men who underwent RP for intermediate-risk PCa at two centers. All men had MRI positive for a PIRADS=3 lesion and a subsequent TBx plus SBx biopsy. All men had PCa with Gleason=7 (GS) in the IL lesion only. PCa foci outside the IL were defined as PCa detected at SBx. We tested the relationship between presence of GS 6 disease outside the IL as well as IL volume and probability of biochemical recurrence (BCR) after RP. Multivariable Cox analysis was used to predict BCR according to IL volume and the presence and extent of GS 3+3 outside IL after accounting for possible confounders. An interaction term between IL volume and TBx GS and loess function assessed the relationship between these two factors in predicting 3-year BCR free survival.
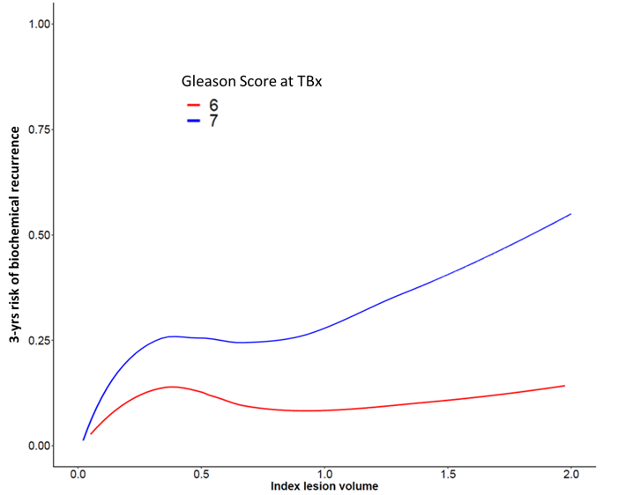
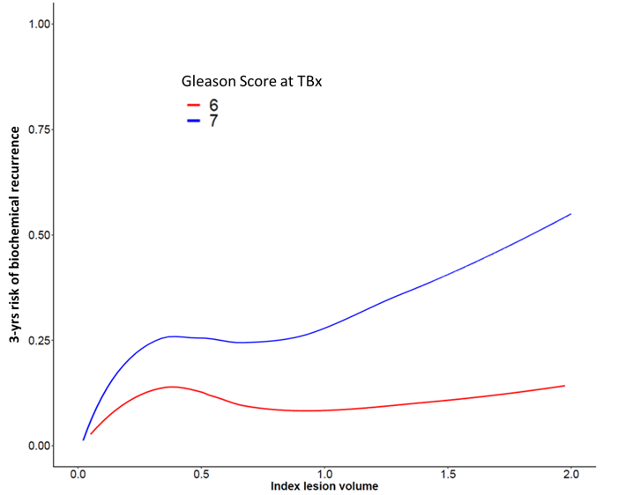
Results: Overall, 80% had GS 3+3 disease outside of the IL while 20% did not have any cancer at systematic biopsy. At MVA, IL volume (HR: 1.2), and PIRADS (HR: 1.5) were predictors of BCR after RP (all p< 0.03). The presence of low-risk disease and its extent outside the IL did not impact on BCR (p=0.2). The interaction term between IL volume and TBx GS was significantly associated with BCR after RP (HR: 1.04, p=0.03). Figure 1 shows that for ILs with GS 6, the 3-years BCR probability was constantly lower than 10% across different IL volumes. On the other hand, for ILs with GS 7, 3-yrs BCR probability significantly increased for IL volume > 1cc
Conclusions: In men with csPCa in the IL only, low risk disease outside the IL did not impact on BCR. In men with IL harboring PCa with GS 7, IL with volume higher than 1 cc were characterised by a non-negligible 3-year risk of BCR. These results should be considered when assessing suitability and extent of FT for patients with a diagnosis of csPCa limited to the mpMRI IL
Source of Funding: None
Methods: We relied on 173 men who underwent RP for intermediate-risk PCa at two centers. All men had MRI positive for a PIRADS=3 lesion and a subsequent TBx plus SBx biopsy. All men had PCa with Gleason=7 (GS) in the IL lesion only. PCa foci outside the IL were defined as PCa detected at SBx. We tested the relationship between presence of GS 6 disease outside the IL as well as IL volume and probability of biochemical recurrence (BCR) after RP. Multivariable Cox analysis was used to predict BCR according to IL volume and the presence and extent of GS 3+3 outside IL after accounting for possible confounders. An interaction term between IL volume and TBx GS and loess function assessed the relationship between these two factors in predicting 3-year BCR free survival.
Results: Overall, 80% had GS 3+3 disease outside of the IL while 20% did not have any cancer at systematic biopsy. At MVA, IL volume (HR: 1.2), and PIRADS (HR: 1.5) were predictors of BCR after RP (all p< 0.03). The presence of low-risk disease and its extent outside the IL did not impact on BCR (p=0.2). The interaction term between IL volume and TBx GS was significantly associated with BCR after RP (HR: 1.04, p=0.03). Figure 1 shows that for ILs with GS 6, the 3-years BCR probability was constantly lower than 10% across different IL volumes. On the other hand, for ILs with GS 7, 3-yrs BCR probability significantly increased for IL volume > 1cc
Conclusions: In men with csPCa in the IL only, low risk disease outside the IL did not impact on BCR. In men with IL harboring PCa with GS 7, IL with volume higher than 1 cc were characterised by a non-negligible 3-year risk of BCR. These results should be considered when assessing suitability and extent of FT for patients with a diagnosis of csPCa limited to the mpMRI IL
Source of Funding: None

.jpg)
.jpg)