Back
Poster, Podium & Video Sessions
MP02: Infections/Inflammation/Cystic Disease of the Genitourinary Tract: Kidney & Bladder I
MP02-13: Is Cystoscopy Indicated in the Evaluation of Female Patients with Recurrent Urinary Tract Infections?
Friday, May 13, 2022
7:00 AM – 8:15 AM
Location: Room 225
Tanner Corse, Linda Dayan, Hunter Hasley*, Nutley, NJ, Simon Gelman, Hackensack, NJ, Debra Fromer, Nutley, NJ
- HH
Poster Presenter(s)
Introduction: According to the 2019 American Urological Association (AUA) guidelines, cystoscopy should not be routinely obtained in the index patient presenting with recurrent urinary tract infection (rUTI). This guideline lacks the support of robust data and is instead based upon expert opinion. We aim to determine the utility of cystoscopy in patients with rUTI in the setting of both uncomplicated and complicated UTI.
Methods: Billing codes were used to identify women who underwent cystoscopy between May 1, 2015 and March 15, 2021 for rUTI (at least 2 culture-proven, symptomatic UTI within 6 months, or 3 within 1 year) at a single tertiary academic medical center. Patients were excluded if they had a competing indication for cystoscopy. Data on risk factors, demographic information, cystoscopic findings, and outcomes of management were analyzed.
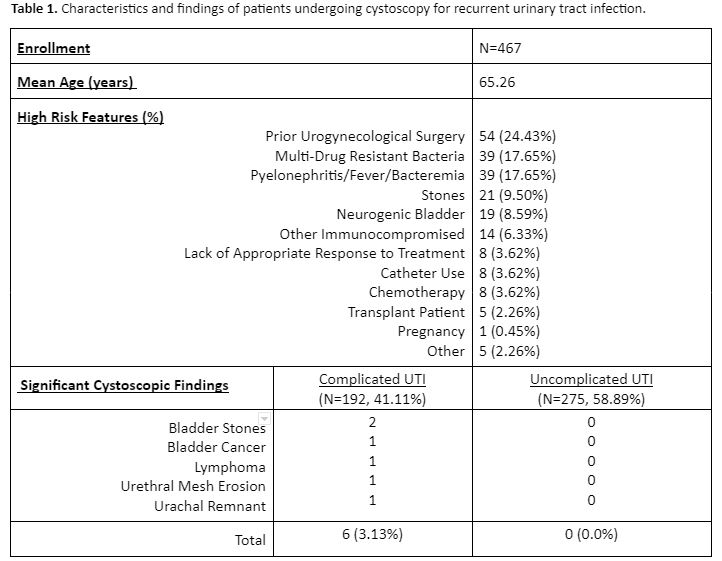
Results: 467 women underwent cystoscopy for rUTI. Demographic data and risk factors are listed in Table 1. 192 (41.11%) were classified as having complicated UTI. In total, only 6 patients (1.28%) were identified with significant cystoscopic findings prompting management that significantly impacted outcome: bladder stones in patients with neurogenic bladder (2), high-grade non-invasive bladder cancer (1), lymphoma (1), urethral erosion of mesh sling (1), and urachal remnant (1). All 6 cases were classified as complicated UTI. 14 patients (2.99%) were found to have mucosal abnormalities prompting cystoscopic biopsy, 3 of which required general anesthesia. Of these, all were benign including findings of cystitis glandularis (1) and papilloma (1). 2 patients (0.42%) were found to have ureteral abnormalities prompting non-diagnostic VCUG.
Conclusions: The diagnostic yield of cystoscopy in women with rUTI is very low, especially in patients with uncomplicated UTI in whom cystoscopy yielded no significant results impacting outcome. Our analysis suggests cystoscopy may have contributed to more invasive testing with limited diagnostic yield.
Source of Funding: None
Methods: Billing codes were used to identify women who underwent cystoscopy between May 1, 2015 and March 15, 2021 for rUTI (at least 2 culture-proven, symptomatic UTI within 6 months, or 3 within 1 year) at a single tertiary academic medical center. Patients were excluded if they had a competing indication for cystoscopy. Data on risk factors, demographic information, cystoscopic findings, and outcomes of management were analyzed.
Results: 467 women underwent cystoscopy for rUTI. Demographic data and risk factors are listed in Table 1. 192 (41.11%) were classified as having complicated UTI. In total, only 6 patients (1.28%) were identified with significant cystoscopic findings prompting management that significantly impacted outcome: bladder stones in patients with neurogenic bladder (2), high-grade non-invasive bladder cancer (1), lymphoma (1), urethral erosion of mesh sling (1), and urachal remnant (1). All 6 cases were classified as complicated UTI. 14 patients (2.99%) were found to have mucosal abnormalities prompting cystoscopic biopsy, 3 of which required general anesthesia. Of these, all were benign including findings of cystitis glandularis (1) and papilloma (1). 2 patients (0.42%) were found to have ureteral abnormalities prompting non-diagnostic VCUG.
Conclusions: The diagnostic yield of cystoscopy in women with rUTI is very low, especially in patients with uncomplicated UTI in whom cystoscopy yielded no significant results impacting outcome. Our analysis suggests cystoscopy may have contributed to more invasive testing with limited diagnostic yield.
Source of Funding: None

.jpg)
.jpg)