Back
Poster, Podium & Video Sessions
MP03: Bladder Cancer: Invasive I
MP03-20: Contemporary Analysis of Cystectomy Complications
Friday, May 13, 2022
7:00 AM – 8:15 AM
Location: Room 222
Kevin Chua*, Hiren Patel, Arnav Srivastava, Sai Krishnaraya Doppalapudi, Benjamin Lichtbroun, Sammy Elsamra, Eric Singer, Thomas Jang, Saum Ghodoussipour, New Brunswick, NJ
Kevin Chua, MD
Resident
Rutgers Robert Wood Johnson Medical School
Poster Presenter(s)
Introduction: Radical cystectomy (RC) is a curative treatment for patients with invasive bladder cancer, but carries significant morbidity. Modern improvements in perioperative care have decreased length of stay (LOS) without effect on complication or readmission rates. Herein, we examine contemporary changes in complication rates of RC.
Methods: The National Surgical Quality Improvement Program (NSQIP) database was queried for RC performed from 2006-2018 for nondisseminated bladder cancer identified by CPT, ICD-9 and 10 codes. Demographics and outcomes were studied across time periods: 2006-2011, 2012-2014 and 2015-2018. 30 day complications were classified as minor (urinary tract infection (UTI), superficial incisional surgical site infection (SSI), pneumonia, blood transfusion) or major (readmission, reoperation, sepsis/septic shock, deep vein thrombosis (DVT), stroke, reintubation, renal failure, myocardial infarction, pulmonary embolus (PE), dehiscence, cardiac arrest, deep incisional SSI, organ/space SSI, death).
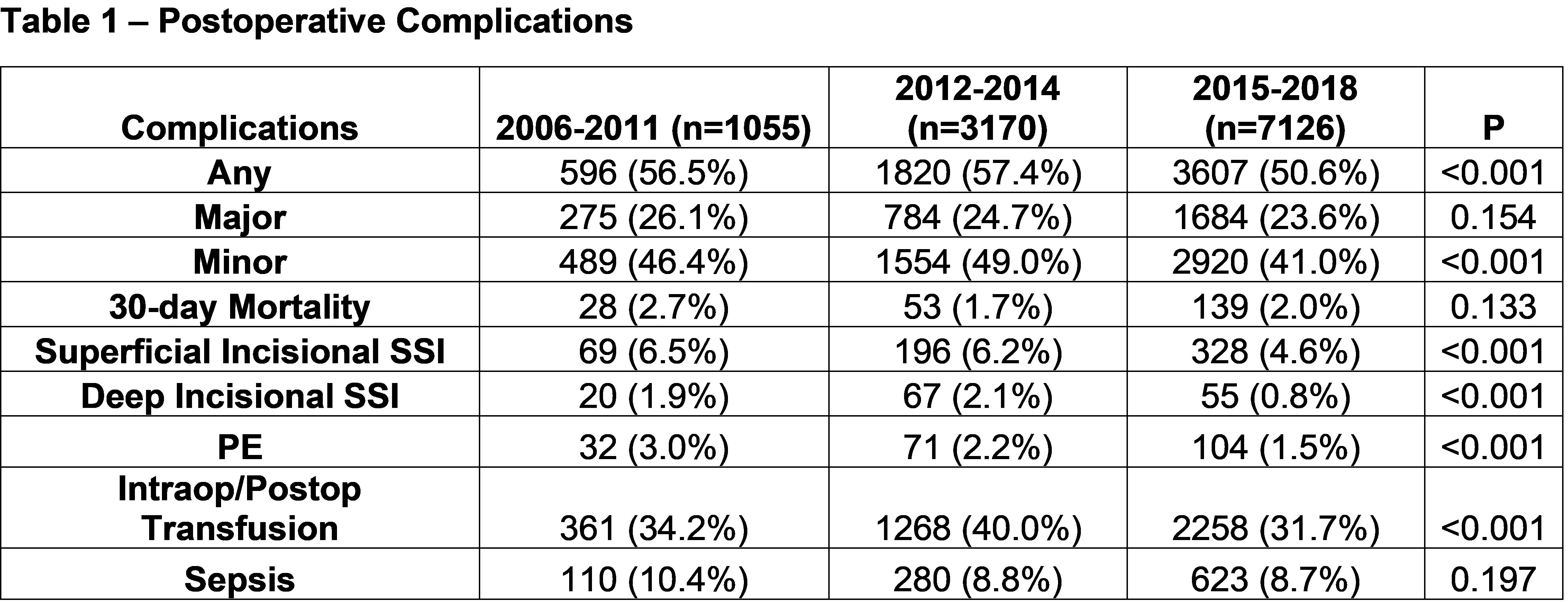
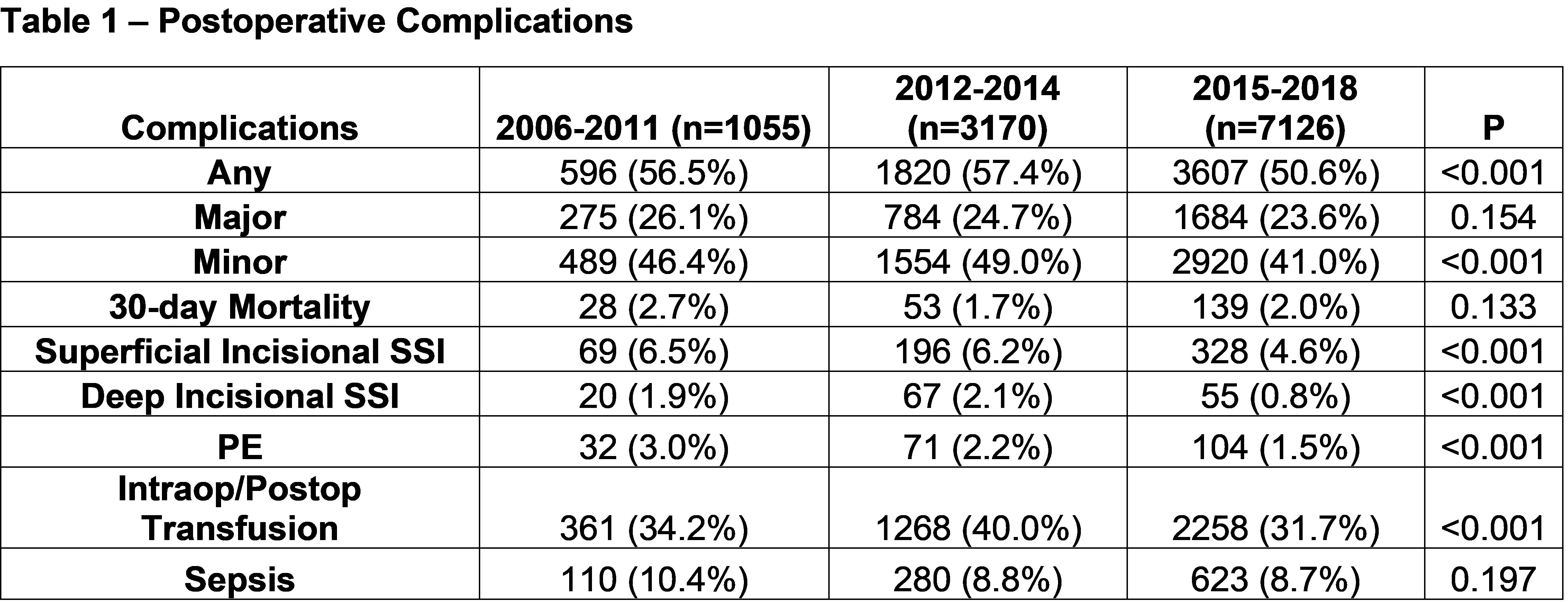
Results: We identified 11,351 RC performed during the study period. Baseline characteristics were similar across the different time periods. Mean length of stay (10.5, 9.8 and 8.6 days, respectively, p<0.001) decreased over time while readmission (20.0, 21.3, and 21.0%, respectively) and mortality rates were stable (2.7, 1.7, 2.0%, respectively). There was a significant decrease in overall minor complications over time, including superficial SSIs and transfusions (Table 1). The rate of major complications decreased over time, though not statistically significantly. Deep SSIs and PEs significantly decreased, while sepsis rates remained stable and high over time (Table 1). Rates of UTI was stable over time (10.1%, 8.8%, 8.3%, respectively, p=0.11).
Conclusions: An analysis of the contemporary era shows continued decrease in LOS after RC and a decrease in overall complications. This may reflect beneficial effects of changes in perioperative bladder cancer management such as increased use of neoadjuvant chemotherapy, enhanced recovery after surgery protocols and laparoscopic/robotic techniques. Further efforts to improve care must target infectious complications and readmissions.
Source of Funding: Grant from the National Cancer Institute (P30CA072720)
Methods: The National Surgical Quality Improvement Program (NSQIP) database was queried for RC performed from 2006-2018 for nondisseminated bladder cancer identified by CPT, ICD-9 and 10 codes. Demographics and outcomes were studied across time periods: 2006-2011, 2012-2014 and 2015-2018. 30 day complications were classified as minor (urinary tract infection (UTI), superficial incisional surgical site infection (SSI), pneumonia, blood transfusion) or major (readmission, reoperation, sepsis/septic shock, deep vein thrombosis (DVT), stroke, reintubation, renal failure, myocardial infarction, pulmonary embolus (PE), dehiscence, cardiac arrest, deep incisional SSI, organ/space SSI, death).
Results: We identified 11,351 RC performed during the study period. Baseline characteristics were similar across the different time periods. Mean length of stay (10.5, 9.8 and 8.6 days, respectively, p<0.001) decreased over time while readmission (20.0, 21.3, and 21.0%, respectively) and mortality rates were stable (2.7, 1.7, 2.0%, respectively). There was a significant decrease in overall minor complications over time, including superficial SSIs and transfusions (Table 1). The rate of major complications decreased over time, though not statistically significantly. Deep SSIs and PEs significantly decreased, while sepsis rates remained stable and high over time (Table 1). Rates of UTI was stable over time (10.1%, 8.8%, 8.3%, respectively, p=0.11).
Conclusions: An analysis of the contemporary era shows continued decrease in LOS after RC and a decrease in overall complications. This may reflect beneficial effects of changes in perioperative bladder cancer management such as increased use of neoadjuvant chemotherapy, enhanced recovery after surgery protocols and laparoscopic/robotic techniques. Further efforts to improve care must target infectious complications and readmissions.
Source of Funding: Grant from the National Cancer Institute (P30CA072720)

.jpg)
.jpg)