Back
Poster, Podium & Video Sessions
MP04: Benign Prostatic Hyperplasia: Surgical Therapy & New Technology II
MP04-05: Increased Bleeding Risk is Associated with 30-day Mortality after TURP
Friday, May 13, 2022
8:45 AM – 10:00 AM
Location: Room 228
Zafardjan Dalimov*, Philadelphia, PA, Ellen Lutnick, Emily C. Ellmann, Ali Houjaij, Nader D. Nader, Oussama M. Darwish, Buffalo, NY

Zafardjan Dalimov, MD, MS
Einstein Healthcare Network
Poster Presenter(s)
Introduction: Transurethral Resection of the Prostate (TURP) is the gold standard of treatment for benign prostatic hyperplasia. Anticoagulant medications are increasingly common in this patient population that carries the risk of bleeding and complications. In this study, we aimed to assess post-operative outcomes after TURP in patient with increased bleeding risk.
Methods: ACS-NSQIP data was queried for patients who underwent TURP between the January 2005 and December 2016. History of bleeding disorder, patients on chronic anticoagulation that was not stopped prior to the surgery, INR above 1.1, PTT above 35 seconds, and platelet counts below 70,000 were used to classify patients as increased bleeding risk. Patients with and without increased bleeding risk were compared in terms of complications, return to operating room, and 30-day mortality. Multivariate logistic regression models were fit to evaluate variables associated with 30-day mortality after TURP. We used chi-square and t-tests for statistical analysis of categorical and continuous variables respectively.
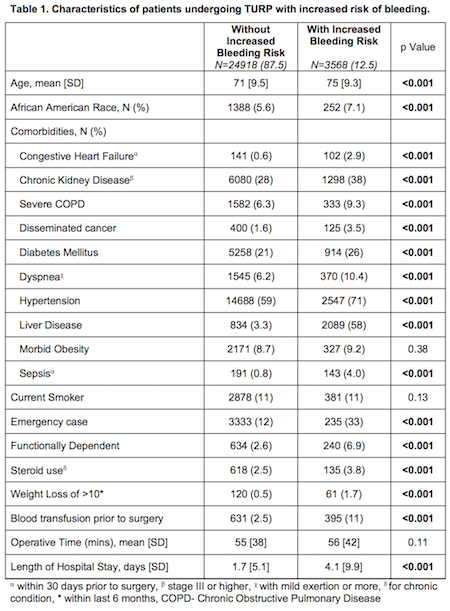
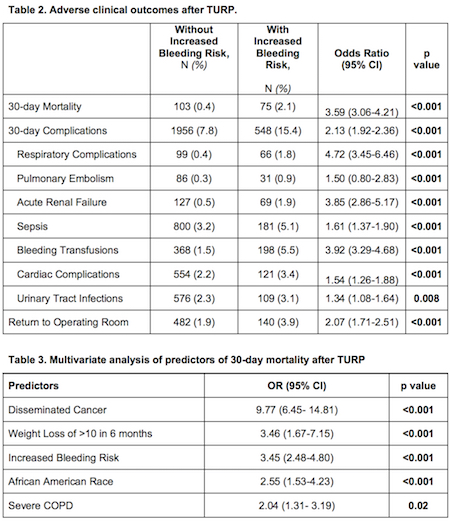
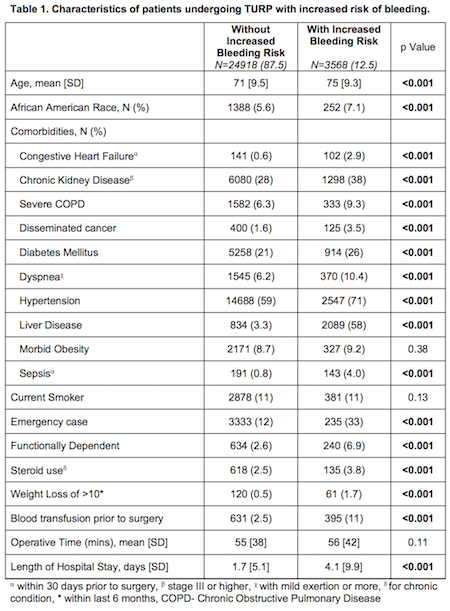
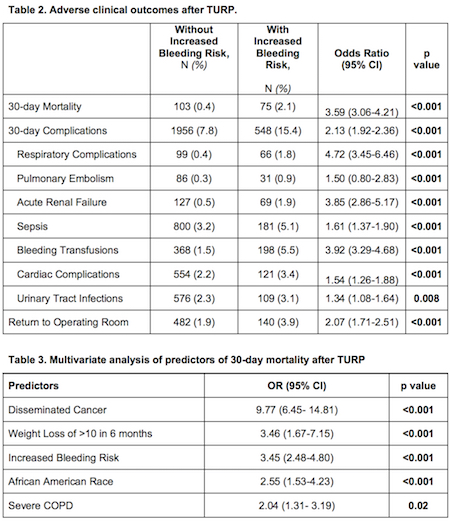
Results: Of the 28,486 patients that underwent TURP, 12.5% were with increased bleeding risk. Patients with increased bleeding risk were older, African American race, had more co-morbidities, functionally dependent, required blood transfusion prior to surgery, more likely to undergo TURP as an emergency case, and had longer hospital stay (Table 1). They had higher 30-day mortality (2.1% vs 0.4%, p<0.001), complications (15.4% vs 7.8%, p<0.001), and re-interventions (3.9% vs 1.9%, p<0.001) (Table 2). On multivariate analysis, disseminated cancer (OR 9.77, p<0.001), significant weight loss (OR 3.46, p<0.001), increased bleeding risk (OR 3.45, p<0.001), African American Race (OR 2.55, p<0.001), and severe COPD (OR 2.04, p=0.02) were associated with mortality within 30 days of TURP (Table 3).
Conclusions: Patients with increased bleeding risk who underwent TURP had more 30-day mortality, complications, and re-operations. Increased bleeding risk was independent predictor of the 30-day mortality.
Source of Funding: N/A
Methods: ACS-NSQIP data was queried for patients who underwent TURP between the January 2005 and December 2016. History of bleeding disorder, patients on chronic anticoagulation that was not stopped prior to the surgery, INR above 1.1, PTT above 35 seconds, and platelet counts below 70,000 were used to classify patients as increased bleeding risk. Patients with and without increased bleeding risk were compared in terms of complications, return to operating room, and 30-day mortality. Multivariate logistic regression models were fit to evaluate variables associated with 30-day mortality after TURP. We used chi-square and t-tests for statistical analysis of categorical and continuous variables respectively.
Results: Of the 28,486 patients that underwent TURP, 12.5% were with increased bleeding risk. Patients with increased bleeding risk were older, African American race, had more co-morbidities, functionally dependent, required blood transfusion prior to surgery, more likely to undergo TURP as an emergency case, and had longer hospital stay (Table 1). They had higher 30-day mortality (2.1% vs 0.4%, p<0.001), complications (15.4% vs 7.8%, p<0.001), and re-interventions (3.9% vs 1.9%, p<0.001) (Table 2). On multivariate analysis, disseminated cancer (OR 9.77, p<0.001), significant weight loss (OR 3.46, p<0.001), increased bleeding risk (OR 3.45, p<0.001), African American Race (OR 2.55, p<0.001), and severe COPD (OR 2.04, p=0.02) were associated with mortality within 30 days of TURP (Table 3).
Conclusions: Patients with increased bleeding risk who underwent TURP had more 30-day mortality, complications, and re-operations. Increased bleeding risk was independent predictor of the 30-day mortality.
Source of Funding: N/A

.jpg)
.jpg)