Back
Poster, Podium & Video Sessions
MP04: Benign Prostatic Hyperplasia: Surgical Therapy & New Technology II
MP04-09: Trends in holmium laser enucleation of the prostate for treatment of benign prostatic hyperplasia
Friday, May 13, 2022
8:45 AM – 10:00 AM
Location: Room 228
Tenny R. Zhang*, Mary O. Strasser, Samantha L. Thorogood, Christina Sze, Bilal Chughtai, Alexis Te, Richard K. Lee, Jim C. Hu, New York, NY
- TZ
Tenny R. Zhang, MD (she/her/hers)
NewYork-Presbyterian/Weill Cornell Medicine
Poster Presenter(s)
Introduction: Compared to traditional treatment options for benign prostatic hyperplasia (BPH), holmium laser enucleation of the prostate (HoLEP) has demonstrated improved outcomes in hemostasis, urinary symptoms, and immediate complication rates. We investigated practice patterns associated with the use of HoLEP.
Methods: We obtained de-identified, self-reported American Board of Urology (ABU) certification/recertification case log data from 2008-2021. We identified 6,632 urologists who performed 73,884 surgeries with an indication for BPH. Current Procedural Terminology (CPT) codes distinguished HoLEP, transurethral resection of prostate (TURP), laser TURP, simple prostatectomy, prostatic urethral lift, transurethral incision of the prostate, and microwave and radiofrequency ablation. We identified 548 urologists (8.3%) who performed 7,386 HoLEP surgeries. Forty-three urologists (0.7%) performed HOLEP exclusively (no other BPH surgical approaches). A logistic regression model was used to determine factors independently associated with using HoLEP.
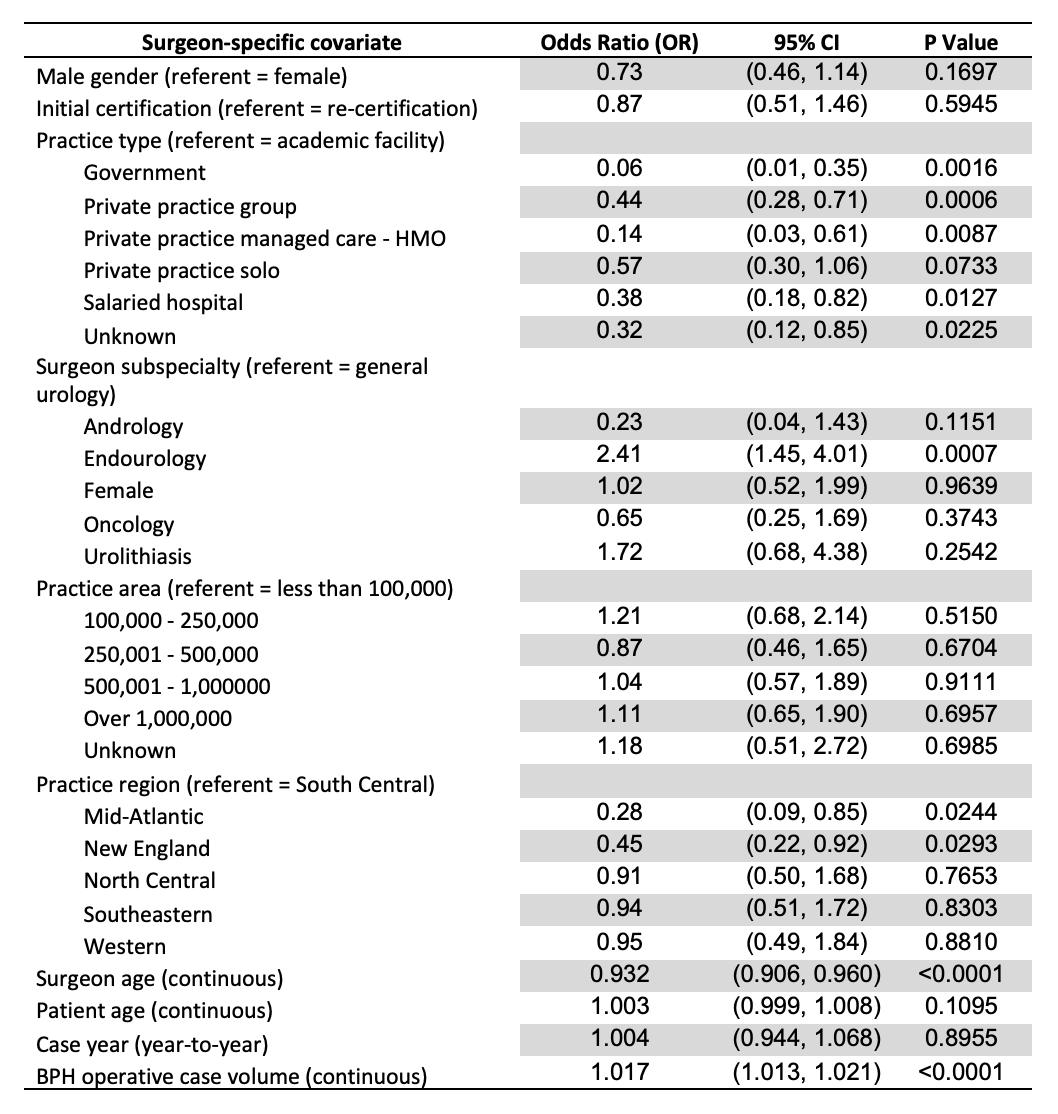
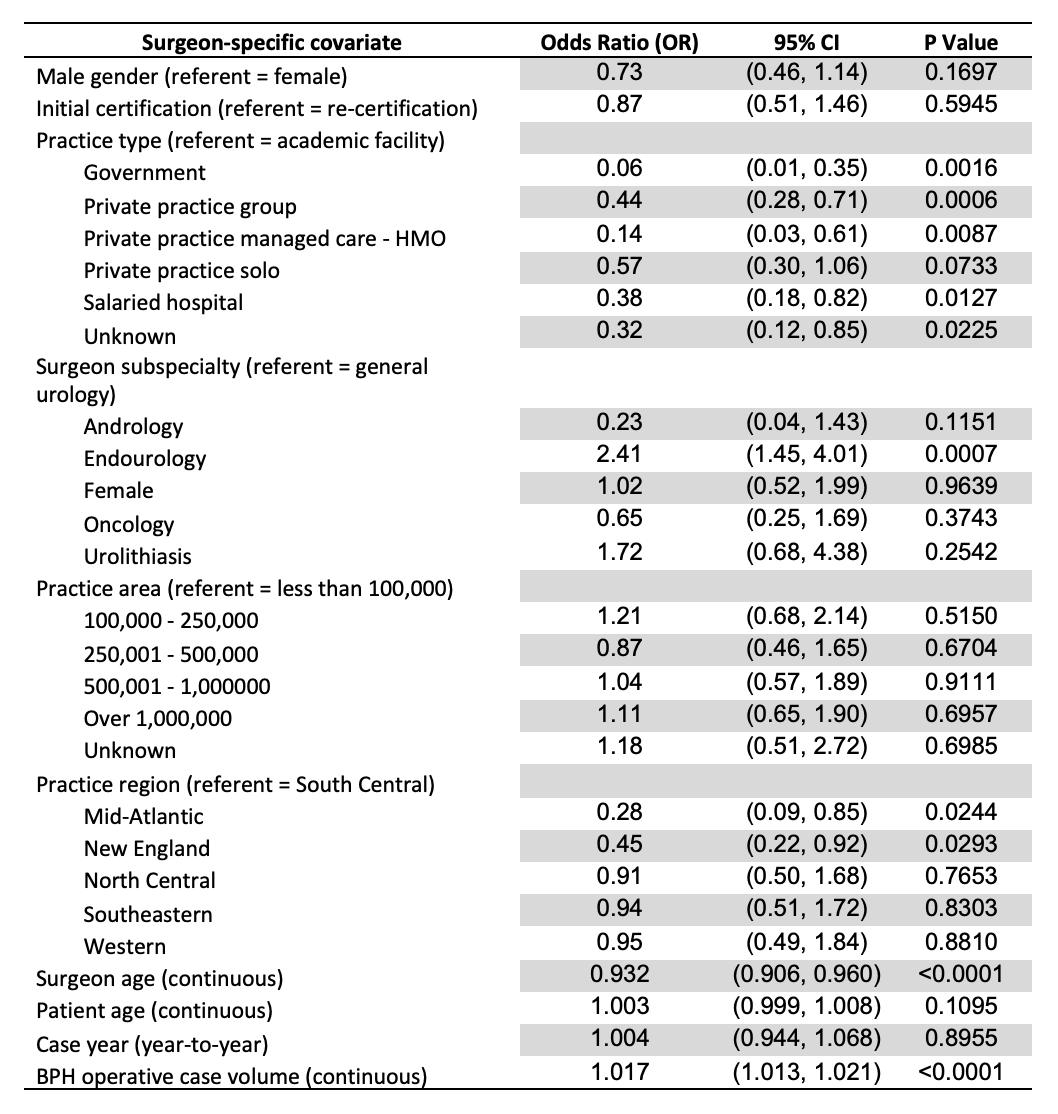
Results: The annual number of HoLEP procedures performed ranged from 3 to 1276, comprising 0.06% to 17.3% of total BPH surgeries annually. Highest HoLEP volumes were logged in 2019, representing 17.3% of total BPH cases. In adjusted analyses (table) factors associated with lower odds of performing HoLEP include surgeon age (odds ratio [OR] 0.93); government (OR 0.06), private practice group (OR 0.44), managed care (OR 0.14), salaried hospital (OR 0.38) vs. academic employment; and Mid-Atlantic (OR 0.28) and New England (0.45) regions vs. South Central (referent). Factors associated with higher odds of performing HoLEP include higher BPH surgical volume (OR 1.02) and endourology (OR 2.41) vs. general urology subspecialty.
Conclusions: HoLEP is more likely to be performed by younger urologists, urologists in academic practice, endourology subspecialists, and those with higher BPH volume. HoLEP was less likely to be performed in Mid-Atlantic and New England regions. Additional studies are needed to elucidate practice pattern variations. Despite evidence demonstrating improved perioperative outcomes compared to competing BPH surgical approaches, HoLEP dissemination over time has been limited, possibly due to prolonged learning curve.
Source of Funding: None.
Methods: We obtained de-identified, self-reported American Board of Urology (ABU) certification/recertification case log data from 2008-2021. We identified 6,632 urologists who performed 73,884 surgeries with an indication for BPH. Current Procedural Terminology (CPT) codes distinguished HoLEP, transurethral resection of prostate (TURP), laser TURP, simple prostatectomy, prostatic urethral lift, transurethral incision of the prostate, and microwave and radiofrequency ablation. We identified 548 urologists (8.3%) who performed 7,386 HoLEP surgeries. Forty-three urologists (0.7%) performed HOLEP exclusively (no other BPH surgical approaches). A logistic regression model was used to determine factors independently associated with using HoLEP.
Results: The annual number of HoLEP procedures performed ranged from 3 to 1276, comprising 0.06% to 17.3% of total BPH surgeries annually. Highest HoLEP volumes were logged in 2019, representing 17.3% of total BPH cases. In adjusted analyses (table) factors associated with lower odds of performing HoLEP include surgeon age (odds ratio [OR] 0.93); government (OR 0.06), private practice group (OR 0.44), managed care (OR 0.14), salaried hospital (OR 0.38) vs. academic employment; and Mid-Atlantic (OR 0.28) and New England (0.45) regions vs. South Central (referent). Factors associated with higher odds of performing HoLEP include higher BPH surgical volume (OR 1.02) and endourology (OR 2.41) vs. general urology subspecialty.
Conclusions: HoLEP is more likely to be performed by younger urologists, urologists in academic practice, endourology subspecialists, and those with higher BPH volume. HoLEP was less likely to be performed in Mid-Atlantic and New England regions. Additional studies are needed to elucidate practice pattern variations. Despite evidence demonstrating improved perioperative outcomes compared to competing BPH surgical approaches, HoLEP dissemination over time has been limited, possibly due to prolonged learning curve.
Source of Funding: None.

.jpg)
.jpg)