Back
Poster, Podium & Video Sessions
MP04: Benign Prostatic Hyperplasia: Surgical Therapy & New Technology II
MP04-14: Patients adhering to standardized protocols for PFMT after HoLEP show higher rates of postoperative incontinence: real-life implications for a rational management work-up
Friday, May 13, 2022
8:45 AM – 10:00 AM
Location: Room 228
Giuseppe Fallara*, Manuela Tutolo, Valentina Specchio, Donatella Giraudo, Shivani Ghazaleh Mathur, Federico Belladelli, Antonio Costa, Daniele Cignoli, Nicolò Schifano, Francesco Pellegrino, Luigi Candela, Mario De Angelis, Gianmarco Colandrea, Milan, Italy, Paolo Capogrosso, Varese, Italy, Eugenio Ventimiglia, Andrea Salonia, Francesco Montorsi, Milan, Italy

Giuseppe Fallara, MD
Università Vita-Salute San Raffaele
Poster Presenter(s)
Introduction: Laser enucleation of the prostate (HoLEP) is associated with a risk of postoperative urinary incontinence (UI). In order to promote early continence recovery, patients might be suggested to perform pelvic floor muscle training (PFMT). We investigated patients’ compliance to postoperative PFMT in patients after HoLEP at a single center.
Methods: The ExpHo trial (NCT03583034) is a prospective observational study collecting data of patients submitted to HoLEP at a single center. Surgeries were performed by a single highly experienced surgeon. Before surgery, all patients completed the International Prostate Symptoms Score (IPSS) questionnaire. Each patient was suggested to undergo PFMT after surgery supervised by a dedicated pelvic floor muscle expert within one month from surgery (in order to standardize PFMT protocols). Compliance to PFMT was assessed. Continence was defined as 0 pads or one security pad. Logistic regression analyses tested the profile of patients who were more likely to comply with PFMT.
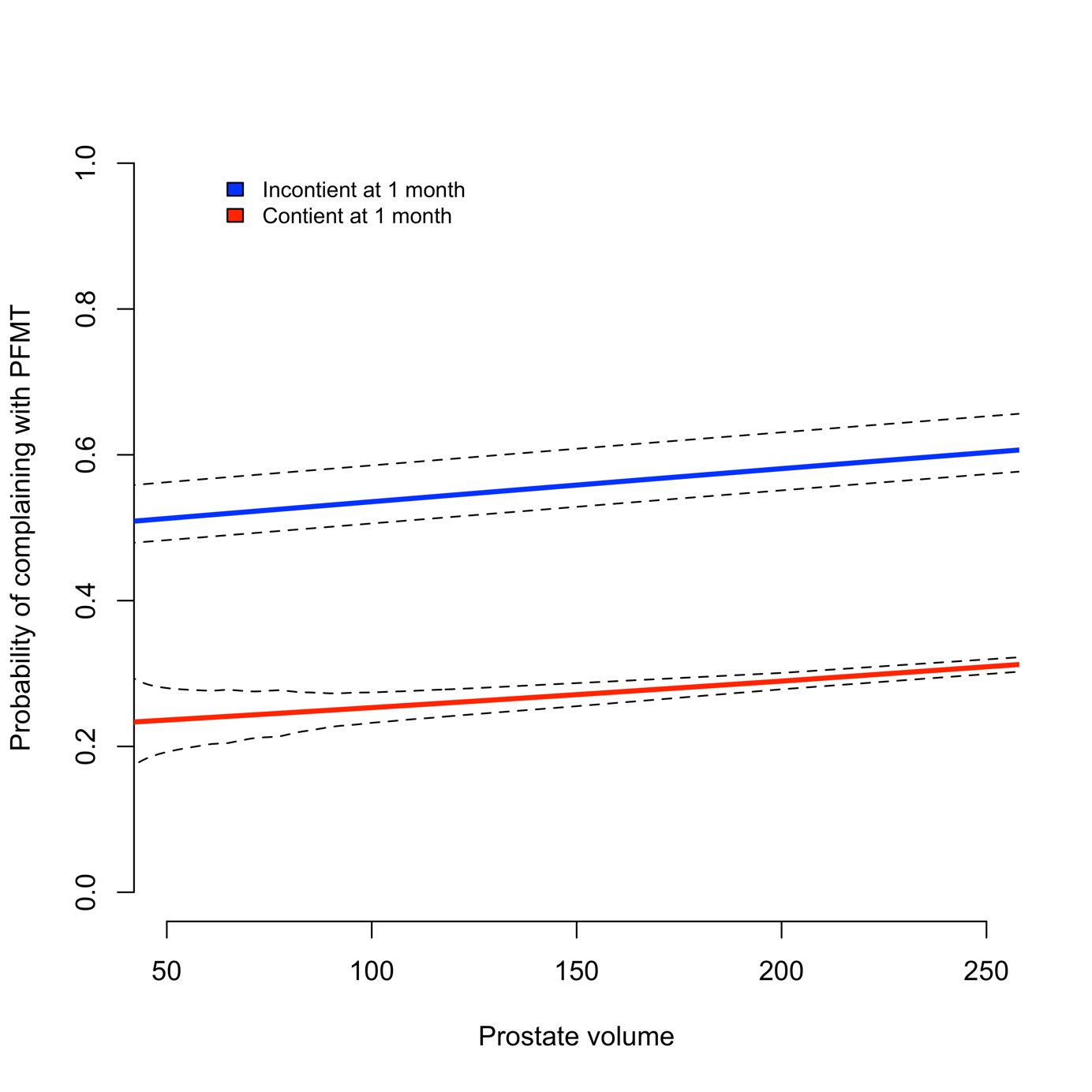
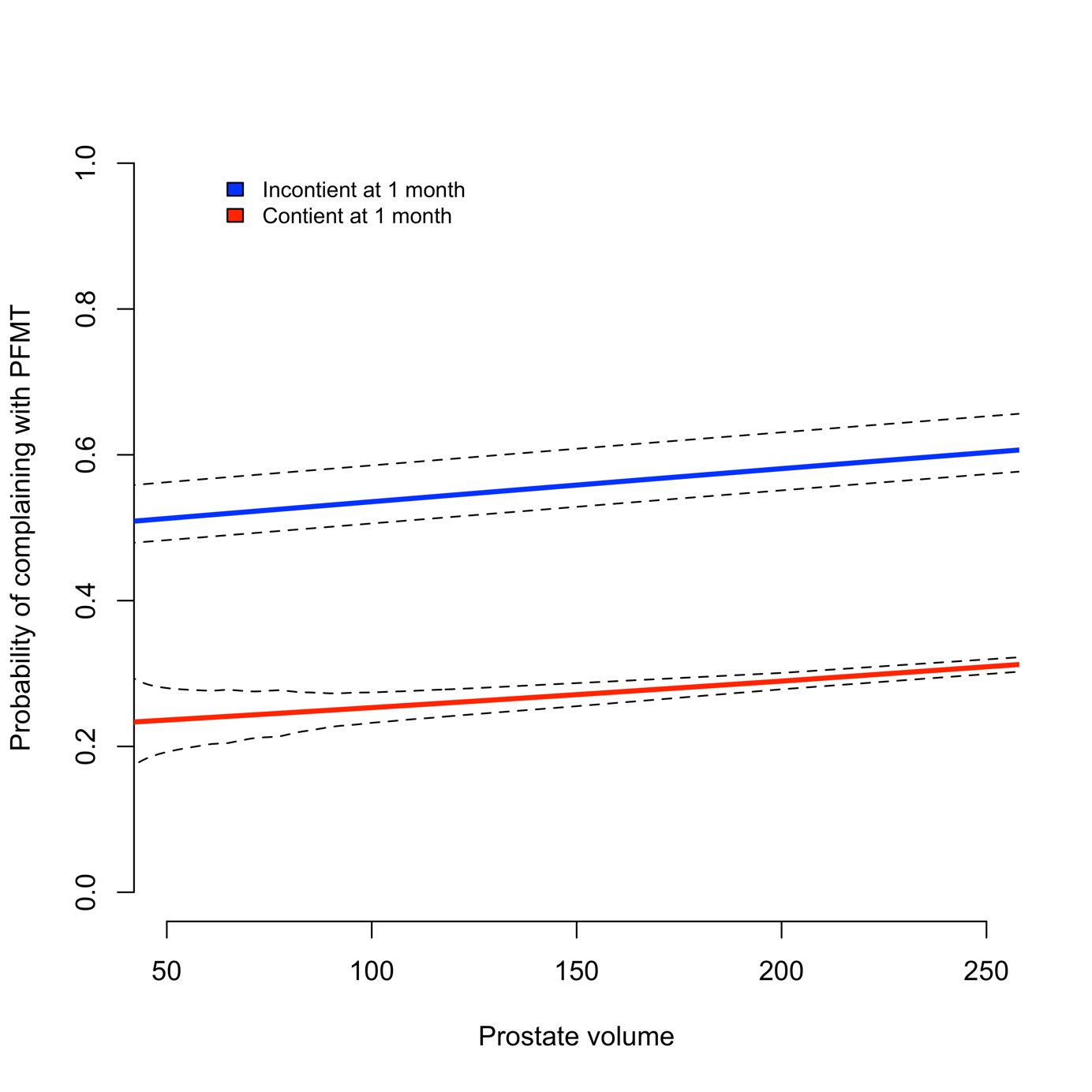
Results: Data were available for 259 patients. Of all, 96 (37%) patients underwent at least one cycle of postoperative PFMT. Patients who underwent PFMT did report more frequently UI at 1 month after surgery (57 [59.4%] vs. 44 [27.0%]; p<0.001). Conversely, patients who did vs. those who did not perform PFMT were comparable in terms of age, prostate volume, baseline IPSS and preoperative uroflowmetry parameters. Likewise, operative time, median discharge time and complication rates were comparable between groups. At logistic regression analysis, patients with greater prostate volume (OR: 1.02; 95%CI: 1.01-1.12; p=0.04) and those who had postoperative UI at 1 month after HoLEP (OR: 3.41, 1.88-6.27; p<0.001) emerged to be more likely to comply with indication for PFMT (Figure 1).
Conclusions: To the best of our knowledge there are no studies assessing the relationship between functional outcomes and the compliance to PFMT in postHoLEP patients. Current findings show that less than half of patients submitted to HoLEP is compliant with the suggestion to perform PFMT. Patients with greater prostate volume and complaining of postoperative incontinence are more likely to comply with this indication.
Source of Funding: no
Methods: The ExpHo trial (NCT03583034) is a prospective observational study collecting data of patients submitted to HoLEP at a single center. Surgeries were performed by a single highly experienced surgeon. Before surgery, all patients completed the International Prostate Symptoms Score (IPSS) questionnaire. Each patient was suggested to undergo PFMT after surgery supervised by a dedicated pelvic floor muscle expert within one month from surgery (in order to standardize PFMT protocols). Compliance to PFMT was assessed. Continence was defined as 0 pads or one security pad. Logistic regression analyses tested the profile of patients who were more likely to comply with PFMT.
Results: Data were available for 259 patients. Of all, 96 (37%) patients underwent at least one cycle of postoperative PFMT. Patients who underwent PFMT did report more frequently UI at 1 month after surgery (57 [59.4%] vs. 44 [27.0%]; p<0.001). Conversely, patients who did vs. those who did not perform PFMT were comparable in terms of age, prostate volume, baseline IPSS and preoperative uroflowmetry parameters. Likewise, operative time, median discharge time and complication rates were comparable between groups. At logistic regression analysis, patients with greater prostate volume (OR: 1.02; 95%CI: 1.01-1.12; p=0.04) and those who had postoperative UI at 1 month after HoLEP (OR: 3.41, 1.88-6.27; p<0.001) emerged to be more likely to comply with indication for PFMT (Figure 1).
Conclusions: To the best of our knowledge there are no studies assessing the relationship between functional outcomes and the compliance to PFMT in postHoLEP patients. Current findings show that less than half of patients submitted to HoLEP is compliant with the suggestion to perform PFMT. Patients with greater prostate volume and complaining of postoperative incontinence are more likely to comply with this indication.
Source of Funding: no

.jpg)
.jpg)