Back
Poster, Podium & Video Sessions
Best Poster Award
MP04: Benign Prostatic Hyperplasia: Surgical Therapy & New Technology II
MP04-19: Single-port Transvesical vs Multiport Robotic Simple Prostatectomy: A Multi-Institutional Matched-pair Comparison
Friday, May 13, 2022
8:45 AM – 10:00 AM
Location: Room 228
Mahmoud Abou Zeinab*, Cleveland, OH, Tanner Corse, Hackensack, NJ, Kennedy Okhawere, New York, NY, Luca Morgantini, Chicago, IL, Nour Abdallah, Alp T. Beksac, Ethan Ferguson, Aaron Kaviani, Joao Pedro Emrich Accioly, Cleveland, OH, Robert Harrison, Bilal Khan, Hackensack, NJ, Indu Saini, Chiya Abramowitz, New York, NY, Susan Talamini, Simone Crivellaro, Chicago, IL, Mutahar Ahmed, Michael Stifelman, Hackensack, NJ, Ketan K. Badani, New York, NY, Jihad Kaouk, Cleveland, OH

Mahmoud Abou Zeinab, MD
Cleveland Clinic
Poster Presenter(s)
Introduction: The introduction of the da Vinci Single Port (SP) robot allowed to perform prostate surgery using the transvesical approach, with promising outcomes. We sought to compare the perioperative outcomes between SP transvesical simple prostatectomy (SP) and multiport simple prostatectomy (MP) in a multi-institutional setting
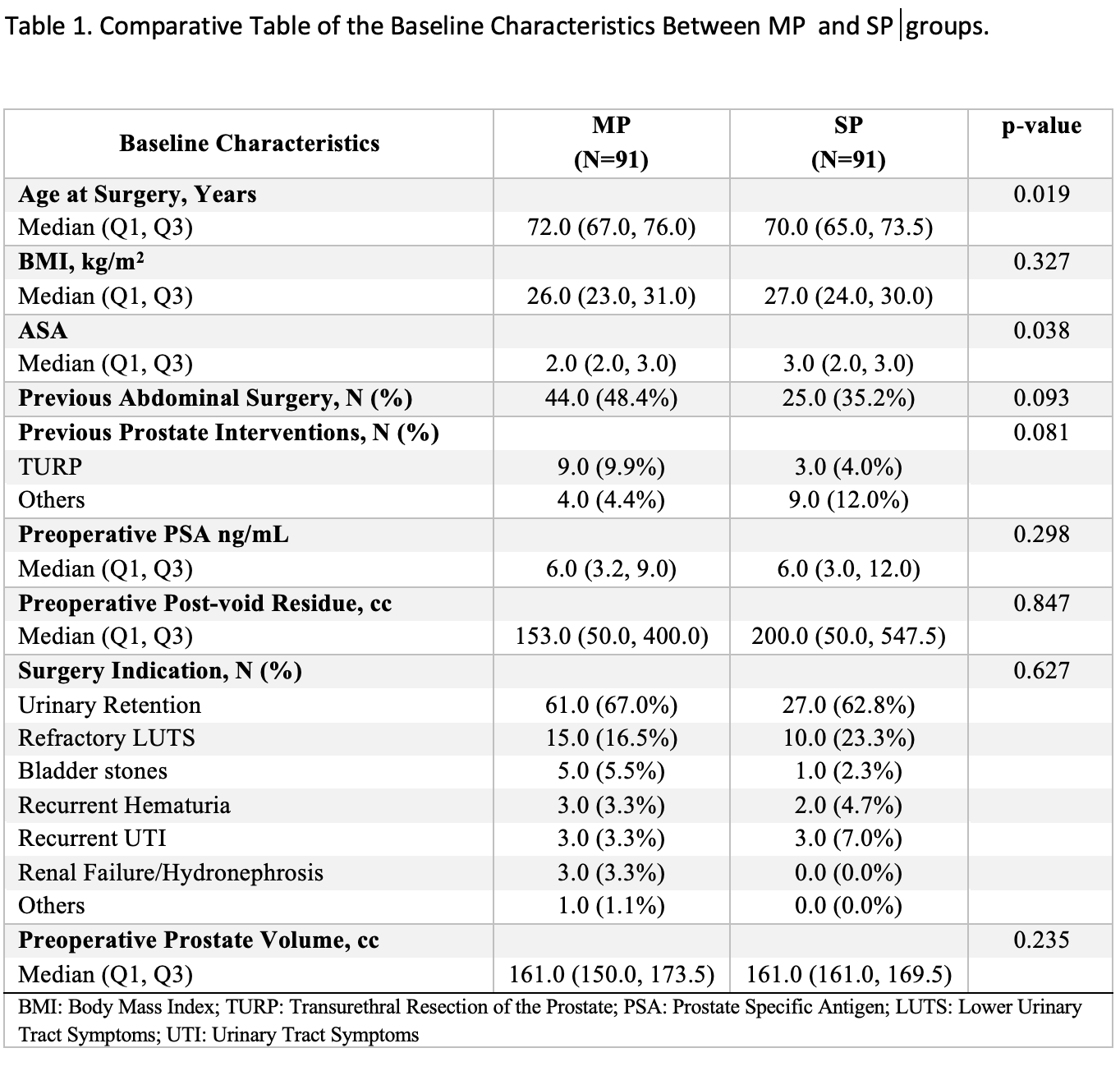
Methods: Prospective data collection of 91 SP patients from February 2020 to October 2021 were collected from three SP centers. Data of 201 patients who underwent MP from January 2017 to October 2021 were retrospectively collected from two separate institutions. All procedures were performed by surgeons with extensive robotic experience. A 1:1 matched-pair analysis for the preoperative prostate volume was performed. Baseline characteristics and perioperative data were analyzed. Mean follow-up was 8 and 5 months for MP and SP, respectively
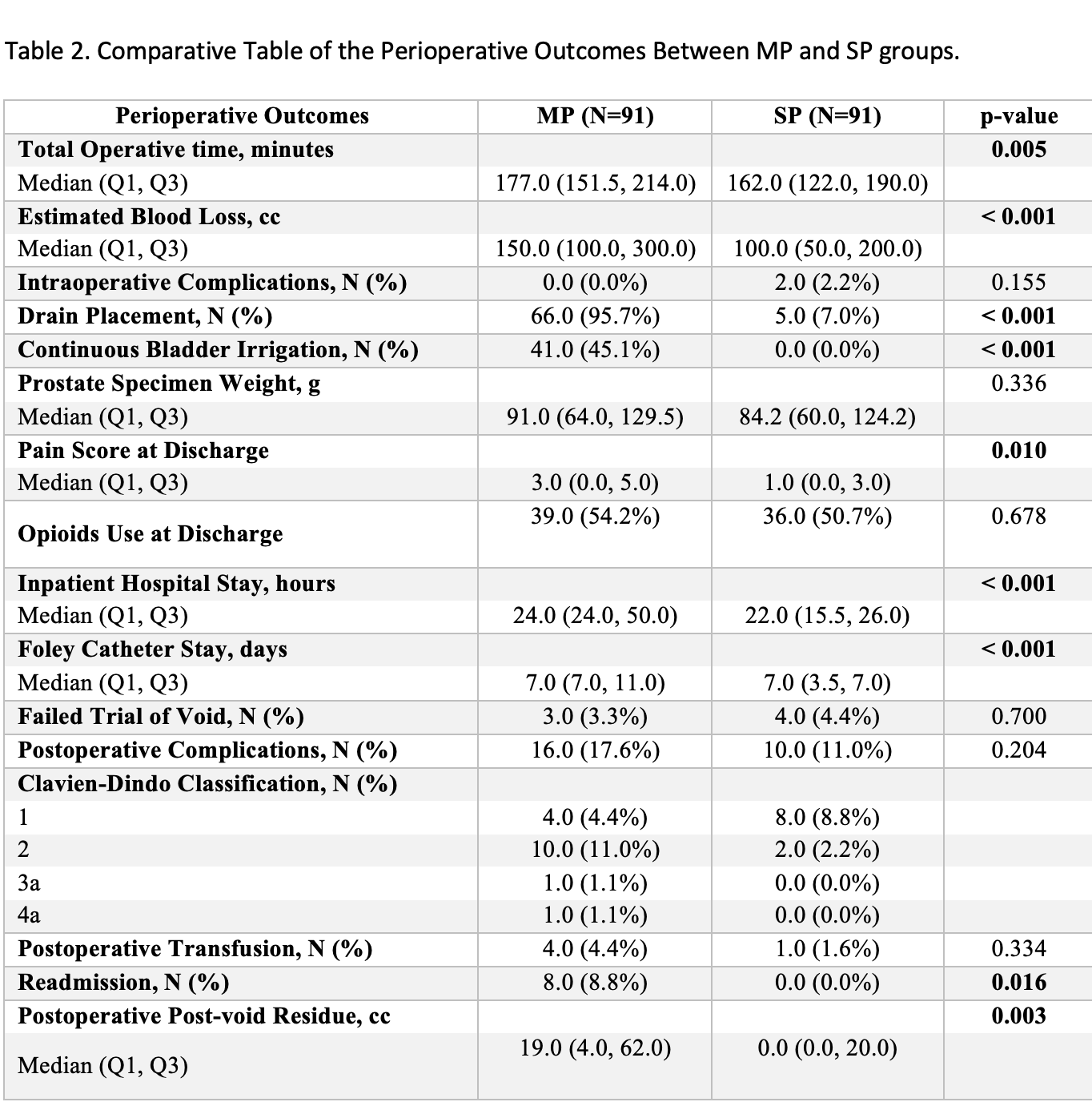
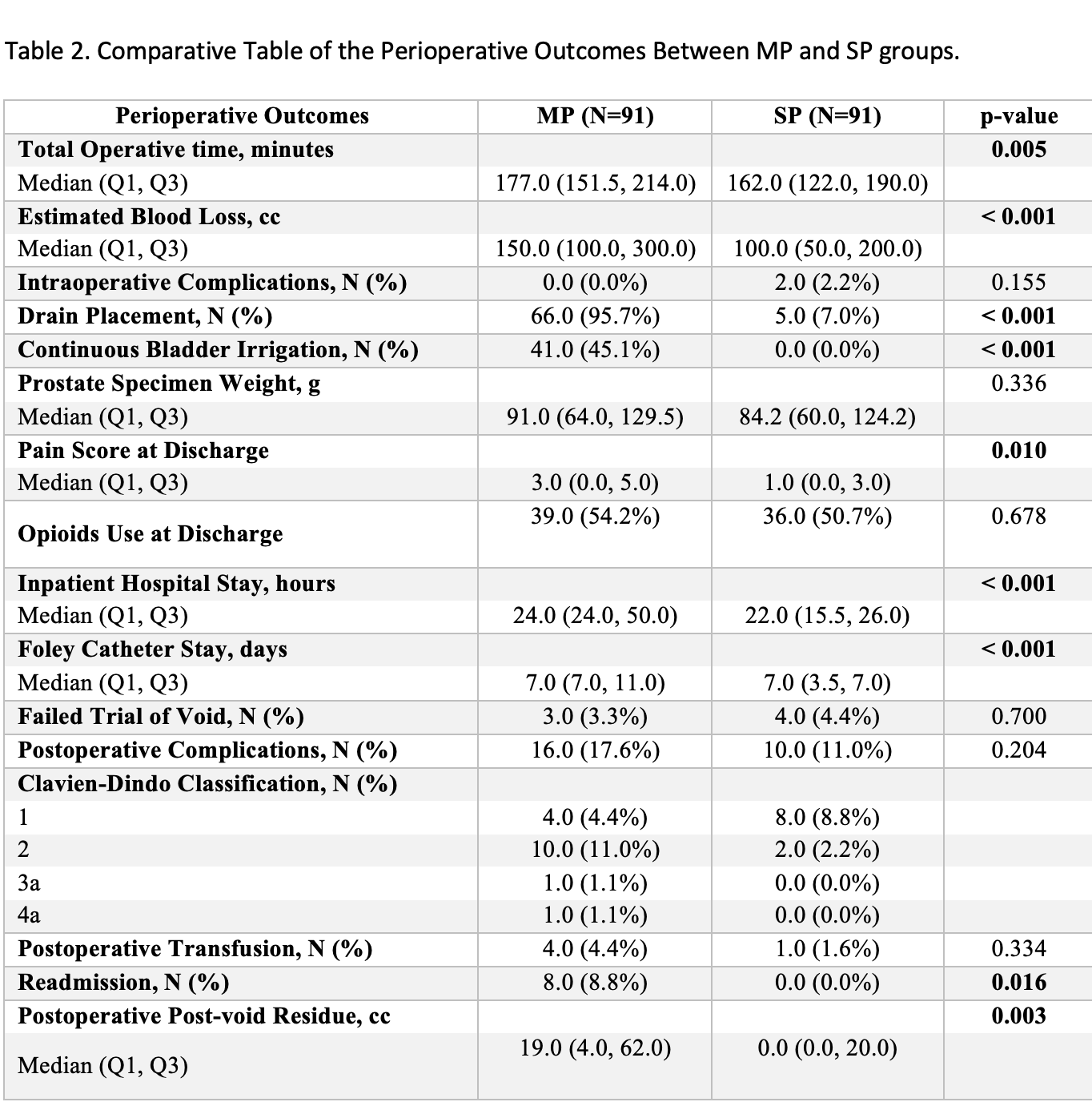
Results: After matching, the median preoperative prostate volume was 161 cc for both groups. Baseline characteristics were comparable. Total operative time was shorter in the SP group (172 vs 162 minutes for MP and SP, respectively, p=.005). Patients in the SP group had less estimated perioperative blood loss, less pelvic drainage, and less continuous bladder irrigation (CBI) (p <.001), however CBI practice varied between centers. There was no difference in the median specimen weight between the two groups. SP patients were more likely to be discharged the same day after the surgery (0 vs 24%, P<.001), with a less median pain score (3 vs 1, P=.010). Both groups had comparable rates of intraoperative or postoperative complications (p=.155 and .204, respectively), however, 8.8% in the MP group got readmitted after surgery compared to 0% in the other group (p=.016).
Conclusions: In experienced hands, SP simple prostatectomy is a good alternative to the MP approach. It allows for shorter hospital stay, less pain on discharge, and potential shorter Foley catheter stay, with no perioperative or functional compromise
Source of Funding: none
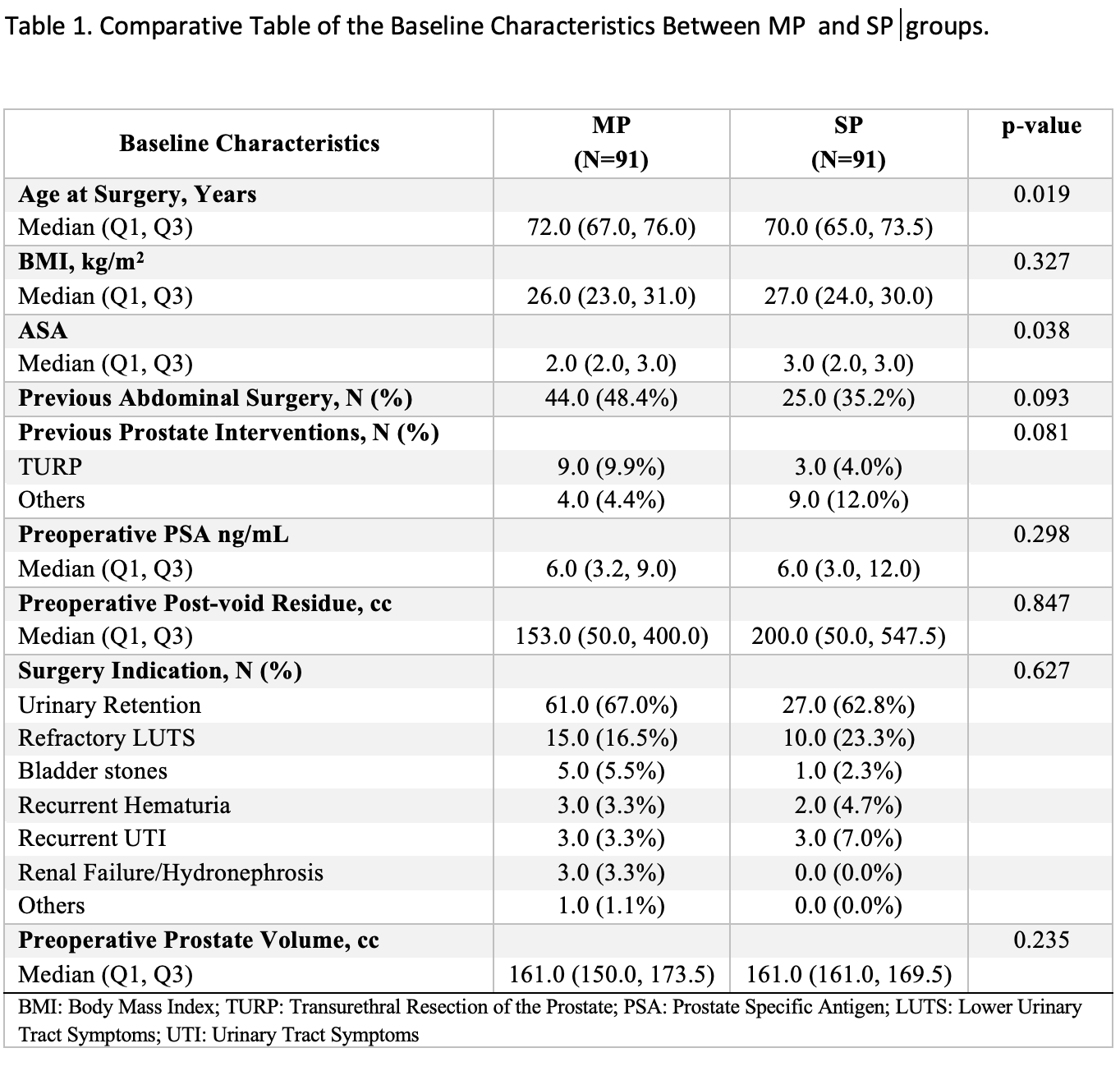
Methods: Prospective data collection of 91 SP patients from February 2020 to October 2021 were collected from three SP centers. Data of 201 patients who underwent MP from January 2017 to October 2021 were retrospectively collected from two separate institutions. All procedures were performed by surgeons with extensive robotic experience. A 1:1 matched-pair analysis for the preoperative prostate volume was performed. Baseline characteristics and perioperative data were analyzed. Mean follow-up was 8 and 5 months for MP and SP, respectively
Results: After matching, the median preoperative prostate volume was 161 cc for both groups. Baseline characteristics were comparable. Total operative time was shorter in the SP group (172 vs 162 minutes for MP and SP, respectively, p=.005). Patients in the SP group had less estimated perioperative blood loss, less pelvic drainage, and less continuous bladder irrigation (CBI) (p <.001), however CBI practice varied between centers. There was no difference in the median specimen weight between the two groups. SP patients were more likely to be discharged the same day after the surgery (0 vs 24%, P<.001), with a less median pain score (3 vs 1, P=.010). Both groups had comparable rates of intraoperative or postoperative complications (p=.155 and .204, respectively), however, 8.8% in the MP group got readmitted after surgery compared to 0% in the other group (p=.016).
Conclusions: In experienced hands, SP simple prostatectomy is a good alternative to the MP approach. It allows for shorter hospital stay, less pain on discharge, and potential shorter Foley catheter stay, with no perioperative or functional compromise
Source of Funding: none

.jpg)
.jpg)