Back
Poster, Podium & Video Sessions
Moderated Poster
MP05: Stone Disease: Basic Research & Pathophysiology
MP05-03: Hypoxia-inducible prolyl hydroxylase inhibitor (Roxadustat) suppresses kidney stone formation.
Friday, May 13, 2022
8:45 AM – 10:00 AM
Location: Room 225
Kengo Kawase*, Shuzo hamamoto, Tatsuya Hattori, Ryosuke chaya, Tomoki Okada, Yutaro Tanaka, Takeru Sugino, Rei Unnno, Kazumi Taguchi, Ryosuke Ando, Atsushi Okada, Takahiro Yasui, Takahiro Yasui, nagoya, Japan
- KK
Poster Presenter(s)
Introduction: In the process of creating a mouse model of kidney stone formation, we discovered that calcium oxalate stones form at the medullary border of the kidney. The anatomy of the medullary border of the kidney is more prone to hypoxia than the other parts of the kidney. In this study, we investigated the effect of a hypoxia-inducible prolyl hydroxylase inhibitor (Roxadustat), which promotes a hypoxic response, on kidney stone formation.
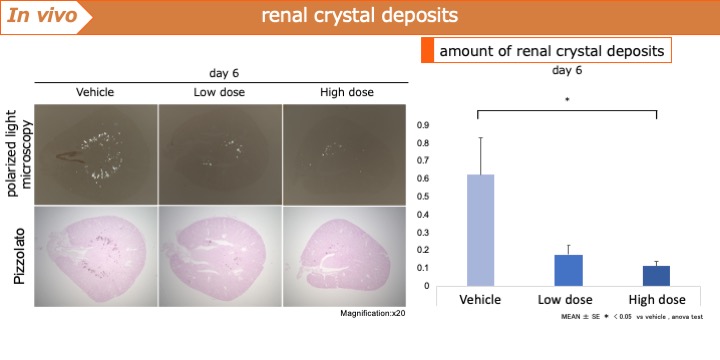
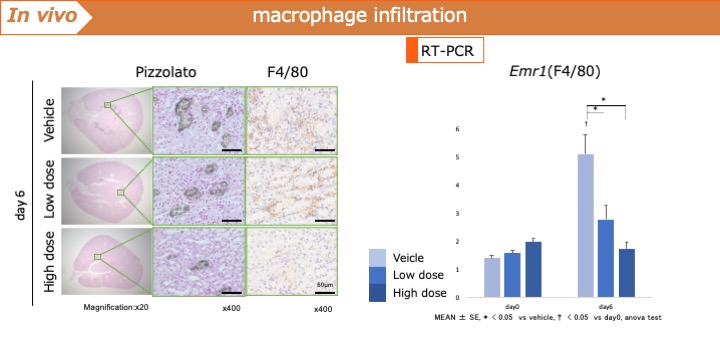
Methods: In vitro: Mouse renal tubular cells were exposed to Roxadustat (0, 25, and 50 µmol/L) for 6 h. Thereafter, calcium oxalate crystals(20 µg/cm2) were added. Inflammation and oxidative stress were determined by quantitative PCR using Ccl2, TNF, Il6, Spp1, and Sod1. Additionally, the extent of crystal adhesion was examined. Next, a negative control group and a group in which siRNA was used to knock down Hif1a was then created and Roxadustat was administered to both groups and the same parameters were studied.In vivo: A PBS-treated group and a Roxadustat-treated group (5 mg, 10 mg/kg/day) were administered to C57BL/6J mice, and 80 mg/kg of glyoxylic acid was administered for 6 days. Stone formation was measured by polarized light microscopy, and Ccl2, Il6, Tnf, Sod1, and Spp1 were examined by PCR. In addition, macrophage infiltration was evaluated by immunostaining for F4/80, a macrophage surface antigen, and PCR for Emr1.
Results: In vitro, Ccl2 and Spp1 were significantly suppressed by Roxadustat, and crystal adhesion was decreased as well. In contrast, knockdown of Hif1a increased Ccl2 and Spp1 and significantly increased crystal adhesion. In vivo, Roxadustat significantly suppressed stone formation by inhibiting Ccl2 and Spp1. Additionally, the macrophages infiltration was significantly inhibited.
Conclusions: Roxadustat not only exerted anti-inflammatory effects via HIF1a in renal tubular epithelial cells, but also inhibited the formation of kidney stones by suppressing macrophage infiltration into the kidney.
Source of Funding: none.
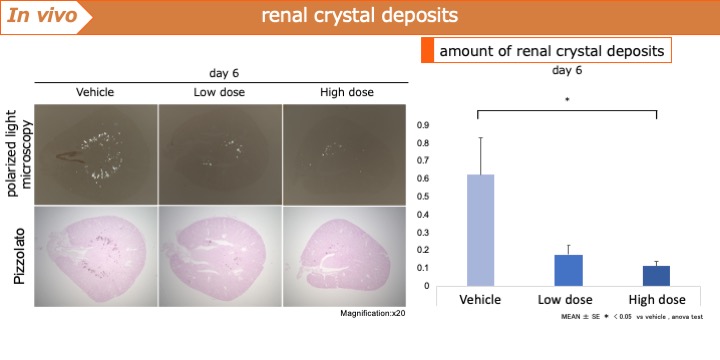
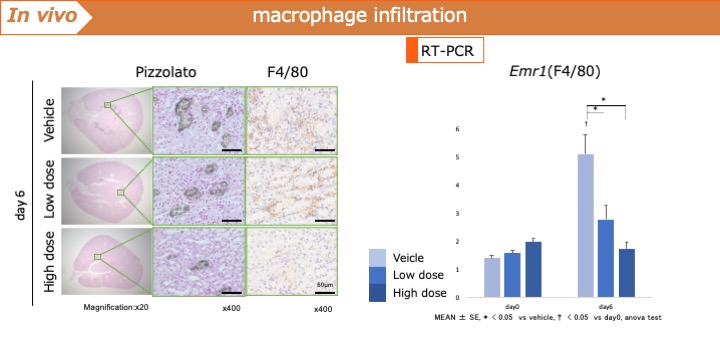
Methods: In vitro: Mouse renal tubular cells were exposed to Roxadustat (0, 25, and 50 µmol/L) for 6 h. Thereafter, calcium oxalate crystals(20 µg/cm2) were added. Inflammation and oxidative stress were determined by quantitative PCR using Ccl2, TNF, Il6, Spp1, and Sod1. Additionally, the extent of crystal adhesion was examined. Next, a negative control group and a group in which siRNA was used to knock down Hif1a was then created and Roxadustat was administered to both groups and the same parameters were studied.In vivo: A PBS-treated group and a Roxadustat-treated group (5 mg, 10 mg/kg/day) were administered to C57BL/6J mice, and 80 mg/kg of glyoxylic acid was administered for 6 days. Stone formation was measured by polarized light microscopy, and Ccl2, Il6, Tnf, Sod1, and Spp1 were examined by PCR. In addition, macrophage infiltration was evaluated by immunostaining for F4/80, a macrophage surface antigen, and PCR for Emr1.
Results: In vitro, Ccl2 and Spp1 were significantly suppressed by Roxadustat, and crystal adhesion was decreased as well. In contrast, knockdown of Hif1a increased Ccl2 and Spp1 and significantly increased crystal adhesion. In vivo, Roxadustat significantly suppressed stone formation by inhibiting Ccl2 and Spp1. Additionally, the macrophages infiltration was significantly inhibited.
Conclusions: Roxadustat not only exerted anti-inflammatory effects via HIF1a in renal tubular epithelial cells, but also inhibited the formation of kidney stones by suppressing macrophage infiltration into the kidney.
Source of Funding: none.

.jpg)
.jpg)