Back
Poster, Podium & Video Sessions
Best Poster Award
MP05: Stone Disease: Basic Research & Pathophysiology
MP05-17: Inflammatory cytokines promote fibrosis in obstructed ureters
Friday, May 13, 2022
8:45 AM – 10:00 AM
Location: Room 225
Alina Reicherz*, Felipe Eltit, Khaled Almutairi, Roman Herout, Michael Cox, Ben Chew, Dirk Lange, Vancouver, Canada
.jpg)
Alina Reicherz, MD
Marien Hospital Herne
Poster Presenter(s)
Introduction: To better understand the impact of ureteral obstruction on ureteral tissue, triggered inflammatory response and fibrotic changes.
Methods: Twenty-four murine ureters were obstructed unilaterally for 7 days. 11 mice were euthanized after clamp removal; 13 mice were recovered after clamp removal for 8 days. Unobstructed ureters from 9 mice served as controls. Peristalsis was determined by magnified observation, and hydronephrosis was evaluated by ultrasound. Ureters were harvested, and ureteral tissue was evaluated histologically. 44 cytokines, chemokines and 5 matrix-metalloproteases were quantified using Multiplex panels (Eve Technologies).
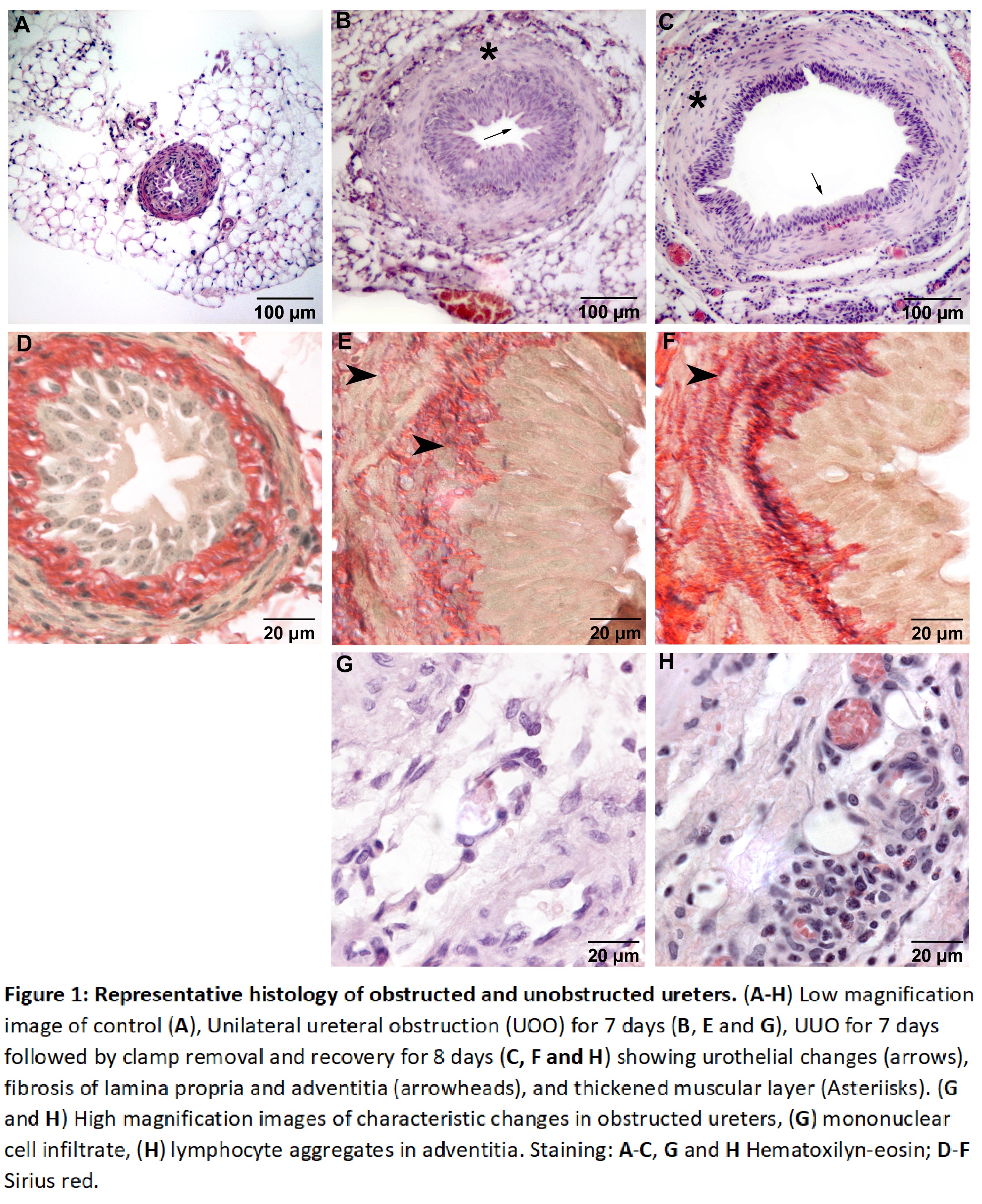
Results: We observed grade 4 hydronephrosis in all obstructed mice. Similarly, peristalsis was reduced significantly and did not recover fully during the 8 days recovery after clamp removal. Histologically, obstructed ureters showed urothelial changes, fibrosis of lamina propria and adventitia, and thickened muscular layers. Collagen fibres infiltrate the muscular layer of all obstructed ureters but are not observed in non-obstructed ureters. Inflammatory changes in the connective tissue of obstructed ureters are characterized by hyperaemia and leukocytes.
Through unsupervised hierarchical clustering, we demonstrate a different cytokine pattern between the groups in which all samples cluster. The highest similarities are observed between the control group and the group of contralateral ureters (ipsilateral side obstructed for 7 days). The group of ureters obstructed for 7 days, and their contralateral ureters are the most different. Consistently, matrix-metalloproteases (MMP-2, MMP-3 and MMP-8) increased significantly after obstruction. Cytokines from T-cell recruitment (IL-16, TARC, MDC) were increased in the obstructed ureter. In addition, the unobstructed, contralateral ureters showed significantly increased levels of cytokines of T-helper cells (Th1: IFN-?, IL-2, IL-12p40, TNFa; Th2: IL-9, IL-10, IL-13).
Conclusions: Ureteral obstruction triggered a pro-inflammatory response and subsequent fibrosis. These changes seem to impair long-term ureteral functionality. Strikingly, the increase of pro-inflammatory cytokines in the contralateral ureters indicates a systemic effect of unilateral ureteral obstruction.
Source of Funding: Alina Reicherz (RE 4611/2-1) is funded by the German Research Foundation (DFG).
Methods: Twenty-four murine ureters were obstructed unilaterally for 7 days. 11 mice were euthanized after clamp removal; 13 mice were recovered after clamp removal for 8 days. Unobstructed ureters from 9 mice served as controls. Peristalsis was determined by magnified observation, and hydronephrosis was evaluated by ultrasound. Ureters were harvested, and ureteral tissue was evaluated histologically. 44 cytokines, chemokines and 5 matrix-metalloproteases were quantified using Multiplex panels (Eve Technologies).
Results: We observed grade 4 hydronephrosis in all obstructed mice. Similarly, peristalsis was reduced significantly and did not recover fully during the 8 days recovery after clamp removal. Histologically, obstructed ureters showed urothelial changes, fibrosis of lamina propria and adventitia, and thickened muscular layers. Collagen fibres infiltrate the muscular layer of all obstructed ureters but are not observed in non-obstructed ureters. Inflammatory changes in the connective tissue of obstructed ureters are characterized by hyperaemia and leukocytes.
Through unsupervised hierarchical clustering, we demonstrate a different cytokine pattern between the groups in which all samples cluster. The highest similarities are observed between the control group and the group of contralateral ureters (ipsilateral side obstructed for 7 days). The group of ureters obstructed for 7 days, and their contralateral ureters are the most different. Consistently, matrix-metalloproteases (MMP-2, MMP-3 and MMP-8) increased significantly after obstruction. Cytokines from T-cell recruitment (IL-16, TARC, MDC) were increased in the obstructed ureter. In addition, the unobstructed, contralateral ureters showed significantly increased levels of cytokines of T-helper cells (Th1: IFN-?, IL-2, IL-12p40, TNFa; Th2: IL-9, IL-10, IL-13).
Conclusions: Ureteral obstruction triggered a pro-inflammatory response and subsequent fibrosis. These changes seem to impair long-term ureteral functionality. Strikingly, the increase of pro-inflammatory cytokines in the contralateral ureters indicates a systemic effect of unilateral ureteral obstruction.
Source of Funding: Alina Reicherz (RE 4611/2-1) is funded by the German Research Foundation (DFG).

.jpg)
.jpg)