Back
Poster, Podium & Video Sessions
Moderated Poster
MP05: Stone Disease: Basic Research & Pathophysiology
MP05-18: Does hypertension affect the recovery of renal functions following reversible unilateral ureteric obstruction?
Friday, May 13, 2022
8:45 AM – 10:00 AM
Location: Room 225
Fayez Hammad*, Loay Lubbad, Al Ain, United Arab Emirates
- FH
Fayez Tawfiq Hammad, MD
United Arab Emirates University
Poster Presenter(s)
Introduction: Both ureteric obstruction (UO) and hypertension are common conditions that might lead to renal functional alterations. The effect of hypertension on the recovery of kidney functions following reversible UO has not been investigated previously. The aim of this study was to investigate the ability of the kidney in hypertensive individuals to recover following reversal of relatively short periods of unilateral ureteric obstruction (UUO) in the rat
Methods: Spontaneously hypertensive (SHT) (n=10) and normotensive Wistar Kyoto (WKY) (n=10) rats underwent 24-hour reversible left UUO. Renal glomerular and tubular functions of the left obstructed (OK) and right non-obstructed (NOK) kidneys were measured using clearance techniques 4 days post-UUO reversal. Gene expression analysis of markers of acute kidney injury and pro-inflammatory and pro-apoptotic cytokines were measured using PCR technique
Results:
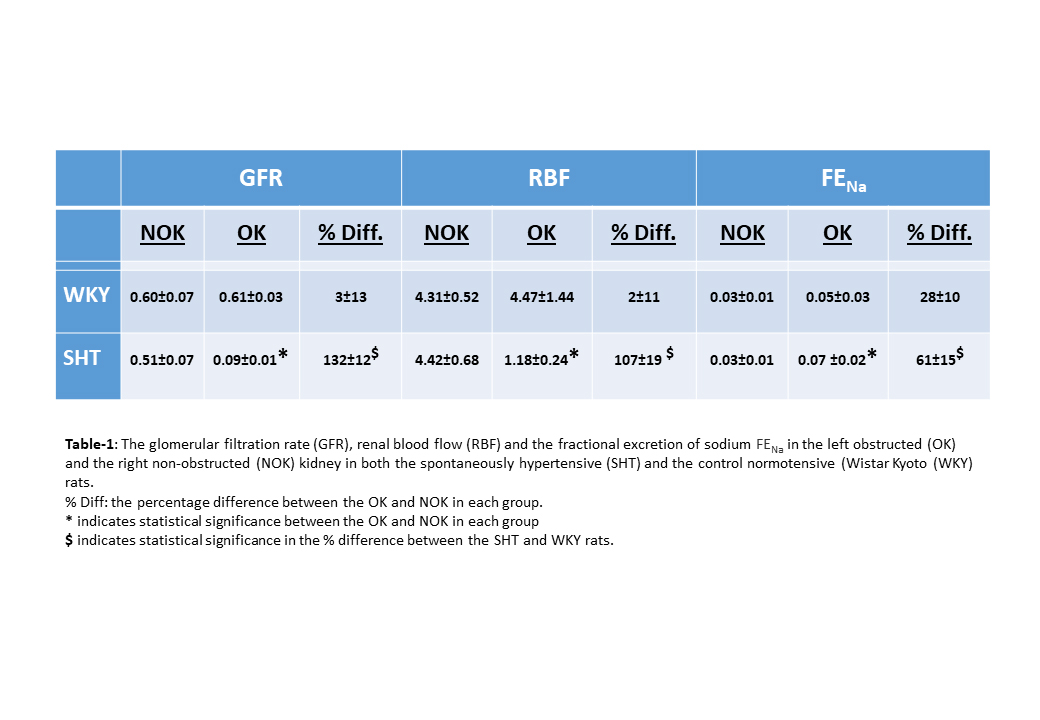
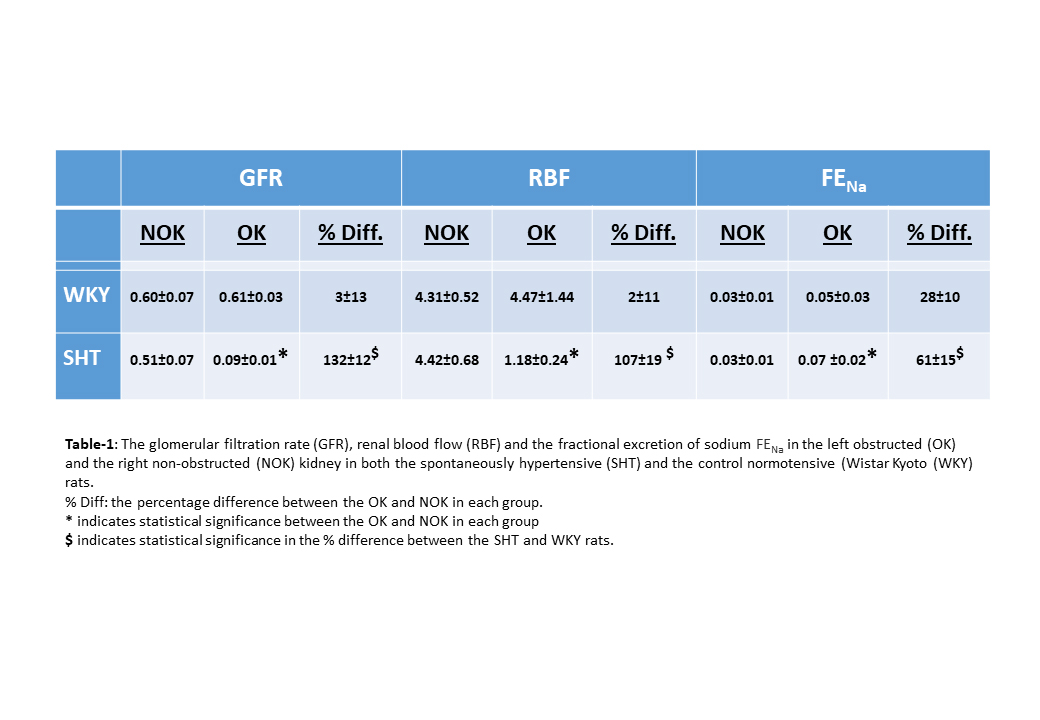
Results: As shown in Table-1, in the WKY rats the glomerular filtration rate, renal blood flow and renal tubular functions such as the fractional excretion of sodium in the OK had returned to normal and were similar to the NOK. However, in the SHT rats, all these parameters in the OK were still severely altered 96 hours following reversal of the UUO as compared to the NOK in the same group. Further, the percentage difference of all the parameters between the OK and NOK in the SHT was significantly higher than the WKY group.
Similarly, hypertension resulted in a significantly higher degree of alterations in the markers of acute kidney injury and in the pro-inflammatory and pro-apoptotic cytokines in the OK. For instance, there was 110±56-fold increase in the gene expression of Kidney Injury Molecule-1 (KIM-1) in the left OK compared to the right NOK in SHT animals compared to 8±3-fold increase in the WKY group (P=0.048). Similarly, the increase in the gene expression of p53 was 1.31±0.08 vs. 1.11±0.05 folds in the SHT and WKY groups, respectively (P=0.036)
Conclusions: Hypertension led to exaggeration in the renal functional alterations associated with UUO. It also caused more pronounced alterations in the acute kidney injury markers and in pro-inflammatory and pro-apoptotic cytokines. These findings might have an impact on the treatment guidelines in hypertensive patients with UUO
Source of Funding: College of Medicine, UAEU
Methods: Spontaneously hypertensive (SHT) (n=10) and normotensive Wistar Kyoto (WKY) (n=10) rats underwent 24-hour reversible left UUO. Renal glomerular and tubular functions of the left obstructed (OK) and right non-obstructed (NOK) kidneys were measured using clearance techniques 4 days post-UUO reversal. Gene expression analysis of markers of acute kidney injury and pro-inflammatory and pro-apoptotic cytokines were measured using PCR technique
Results:
Results: As shown in Table-1, in the WKY rats the glomerular filtration rate, renal blood flow and renal tubular functions such as the fractional excretion of sodium in the OK had returned to normal and were similar to the NOK. However, in the SHT rats, all these parameters in the OK were still severely altered 96 hours following reversal of the UUO as compared to the NOK in the same group. Further, the percentage difference of all the parameters between the OK and NOK in the SHT was significantly higher than the WKY group.
Similarly, hypertension resulted in a significantly higher degree of alterations in the markers of acute kidney injury and in the pro-inflammatory and pro-apoptotic cytokines in the OK. For instance, there was 110±56-fold increase in the gene expression of Kidney Injury Molecule-1 (KIM-1) in the left OK compared to the right NOK in SHT animals compared to 8±3-fold increase in the WKY group (P=0.048). Similarly, the increase in the gene expression of p53 was 1.31±0.08 vs. 1.11±0.05 folds in the SHT and WKY groups, respectively (P=0.036)
Conclusions: Hypertension led to exaggeration in the renal functional alterations associated with UUO. It also caused more pronounced alterations in the acute kidney injury markers and in pro-inflammatory and pro-apoptotic cytokines. These findings might have an impact on the treatment guidelines in hypertensive patients with UUO
Source of Funding: College of Medicine, UAEU

.jpg)
.jpg)