Back
Poster, Podium & Video Sessions
Moderated Poster
MP07: Bladder & Urethra: Anatomy, Physiology & Pharmacology
MP07-11: Real World Medication Persistence in Treatment of Women with Overactive Bladder according to Large Scale Prescription Claims Data
Friday, May 13, 2022
10:30 AM – 11:45 AM
Location: Room 228
Chen Shenhar*, Petah Tikva, Israel, Karin Lifshitz, Igor Mintz, Yariv Shtabholtz, Ofer Yossepowitch, Tel Aviv, Israel, Jack Baniel, Shachar Aharony, Petah Tikva, Israel

Chen Shenhar, MD
Tel Aviv University
Poster Presenter(s)
Introduction: Medical treatments for overactive bladder (OAB) have proven efficacy in controlled trials. However, 1-year medication persistence is reported to be as low as 25% for anticholinergics and 40% for ß3 agonists. Real world data on treatment continuation and sequence in case of medication replacement is limited. Our aim was to study actual treatment persistence trends in women initiated on OAB medications.
Methods: We used advanced data-mining techniques to explore the largest regional provider’s medication purchase database, dispensing for over 400,000 patients, for all women initiating OAB pharmacotherapy between 2010 and 2020, and cross-referenced them with patient age, BMI, and smoking status.
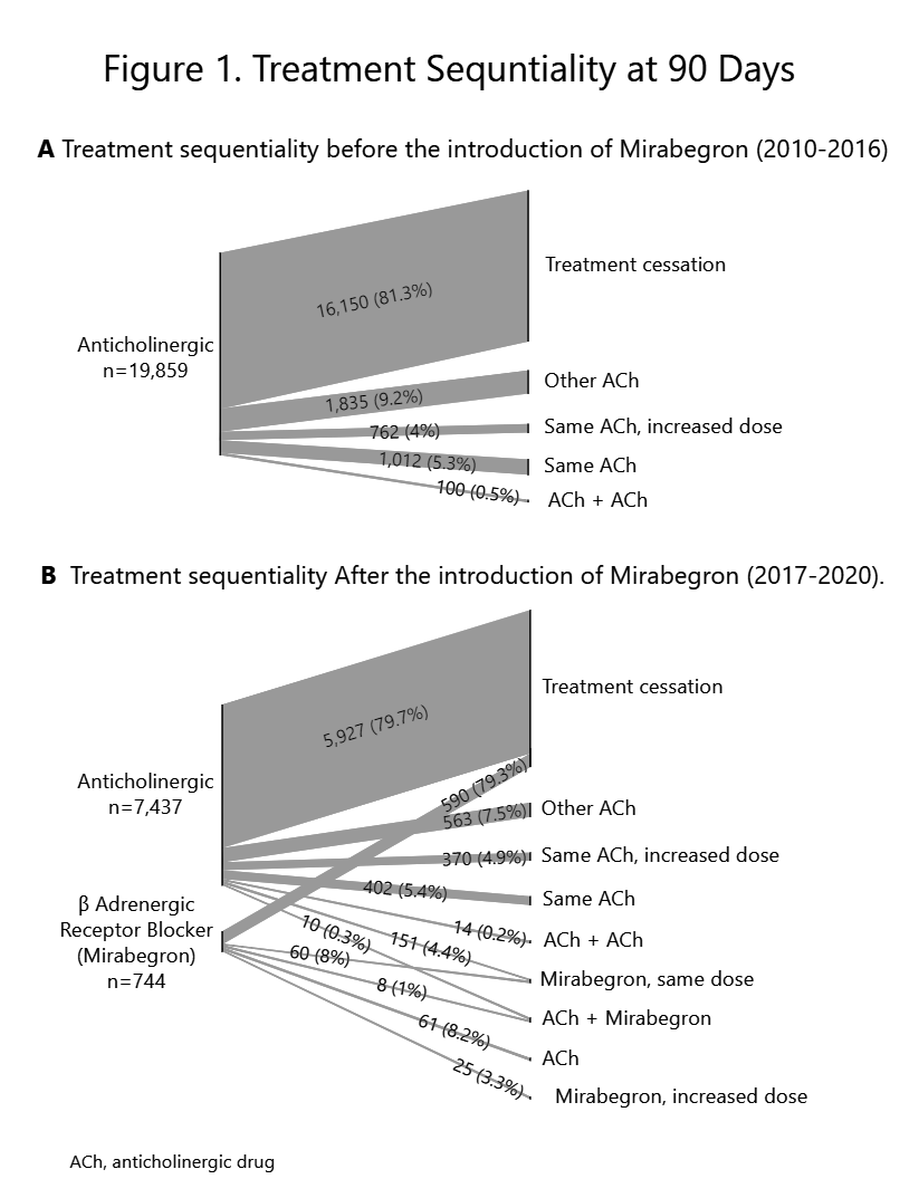
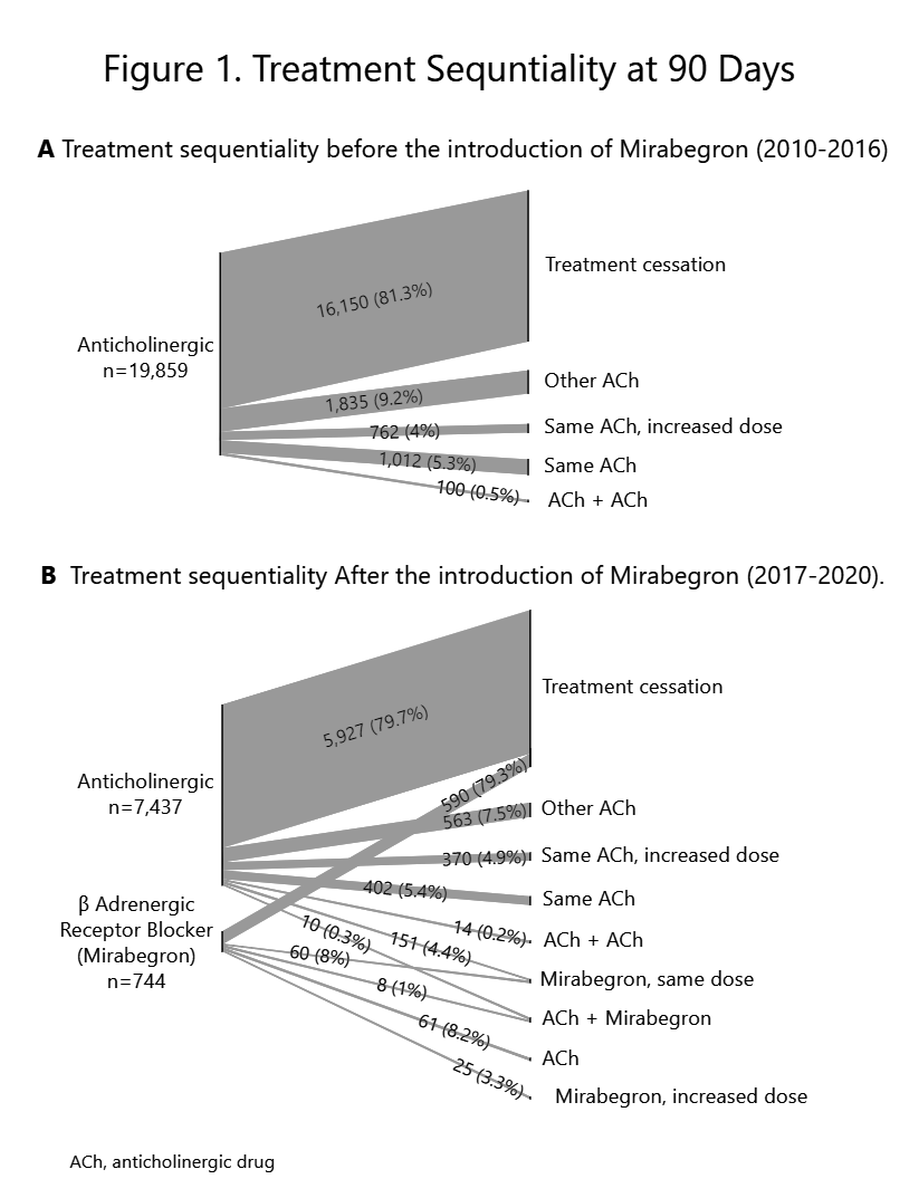
Medication persistence was measured in days for which the patient was issued a medication, and prescription non-refilling for 90 days was defined as non-persistence. We employed a Sankey diagram to map trends in OAB medication claims and treatment sequence. We further compared medication persistence using Kaplan-Meier survival curves and pairwise log-rank analysis. We studied the effects of age and smoking status on medication continuation using logistic regression modelling.
Results: Between 2010 and 2020, 46,079 women made 791,681 unique acquisitions of OAB medications. Overall treatment persistence rates were 49% for 30 days, 34% for 90 days, and 9% for a year. The 1-year persistence rate was highest for Mirabegron (10%) and Oxybutynin (11%) compared with all other medications (4%) (p < 0.005).
Overall persistence rates were unchanged when stratifying by time of Mirabegron acceptance into insurance coverage (p>0.05).
Patients persisting with treatment for over 90 days were 5 years older compared to their non-persisting counterparts (mean age 72.8±14.3 vs. 67.5±16.5 years, p<0.05). Non-smokers had an odds ratio of 1.1 [95% CI: 1.04-1.16] of persistence when compared to smokers.
Conclusions: Real-world OAB pharmacotherapy persistence rates are lower than previously reported. The added option of Mirabegron did not seem to improve these rates.
Source of Funding: none.
Methods: We used advanced data-mining techniques to explore the largest regional provider’s medication purchase database, dispensing for over 400,000 patients, for all women initiating OAB pharmacotherapy between 2010 and 2020, and cross-referenced them with patient age, BMI, and smoking status.
Medication persistence was measured in days for which the patient was issued a medication, and prescription non-refilling for 90 days was defined as non-persistence. We employed a Sankey diagram to map trends in OAB medication claims and treatment sequence. We further compared medication persistence using Kaplan-Meier survival curves and pairwise log-rank analysis. We studied the effects of age and smoking status on medication continuation using logistic regression modelling.
Results: Between 2010 and 2020, 46,079 women made 791,681 unique acquisitions of OAB medications. Overall treatment persistence rates were 49% for 30 days, 34% for 90 days, and 9% for a year. The 1-year persistence rate was highest for Mirabegron (10%) and Oxybutynin (11%) compared with all other medications (4%) (p < 0.005).
Overall persistence rates were unchanged when stratifying by time of Mirabegron acceptance into insurance coverage (p>0.05).
Patients persisting with treatment for over 90 days were 5 years older compared to their non-persisting counterparts (mean age 72.8±14.3 vs. 67.5±16.5 years, p<0.05). Non-smokers had an odds ratio of 1.1 [95% CI: 1.04-1.16] of persistence when compared to smokers.
Conclusions: Real-world OAB pharmacotherapy persistence rates are lower than previously reported. The added option of Mirabegron did not seem to improve these rates.
Source of Funding: none.

.jpg)
.jpg)