Back
Poster, Podium & Video Sessions
Moderated Poster
MP08: Pediatric Urology: Penis & Scrotum
MP08-17: Spinal Anesthesia for Infant Outpatient Genital Surgery
Friday, May 13, 2022
10:30 AM – 11:45 AM
Location: Room 225
Jack Elder*, Andrew Chen, Jacquelin Peck, Christine Mai, Diana Liu, David August, Chang A Liu, Boston, MA

Jack S. Elder, MD
Director of Pediatric Urology
Massachusetts General Hospital
Poster Presenter(s)
Introduction: Spinal anesthesia (SA) avoids the need for endotracheal intubation in general anesthesia (GA), reduces the risk of adverse airway events and avoids intraoperative narcotic administration. We hypothesized that SA is a safe alternative to GA in healthy infants with genital anomalies in the ambulatory setting.
Methods: A prospective IRB-approved database for pediatric patients undergoing urologic surgery under SA was created. Typically, patients < 10 months and < 10 kg are selected for SA. EMLA cream is applied to the L3-L5 interspace for 30 minutes. Patients receive intrathecal plain 0.5% bupivacaine 1 mg/kg without additional sedatives. Clonidine 1 µg/ml is added to extend the duration of the block if the procedure is anticipated to last > 75 minutes. Patients are soothed with a sugar solution and pacifier. Patients receive a caudal block following the procedure for postoperative pain relief. Patient age, gestational age, weight, time to place spinal anesthetic, spinal medication(s) used, surgical procedure, procedure length and peri-anesthetic events were recorded.
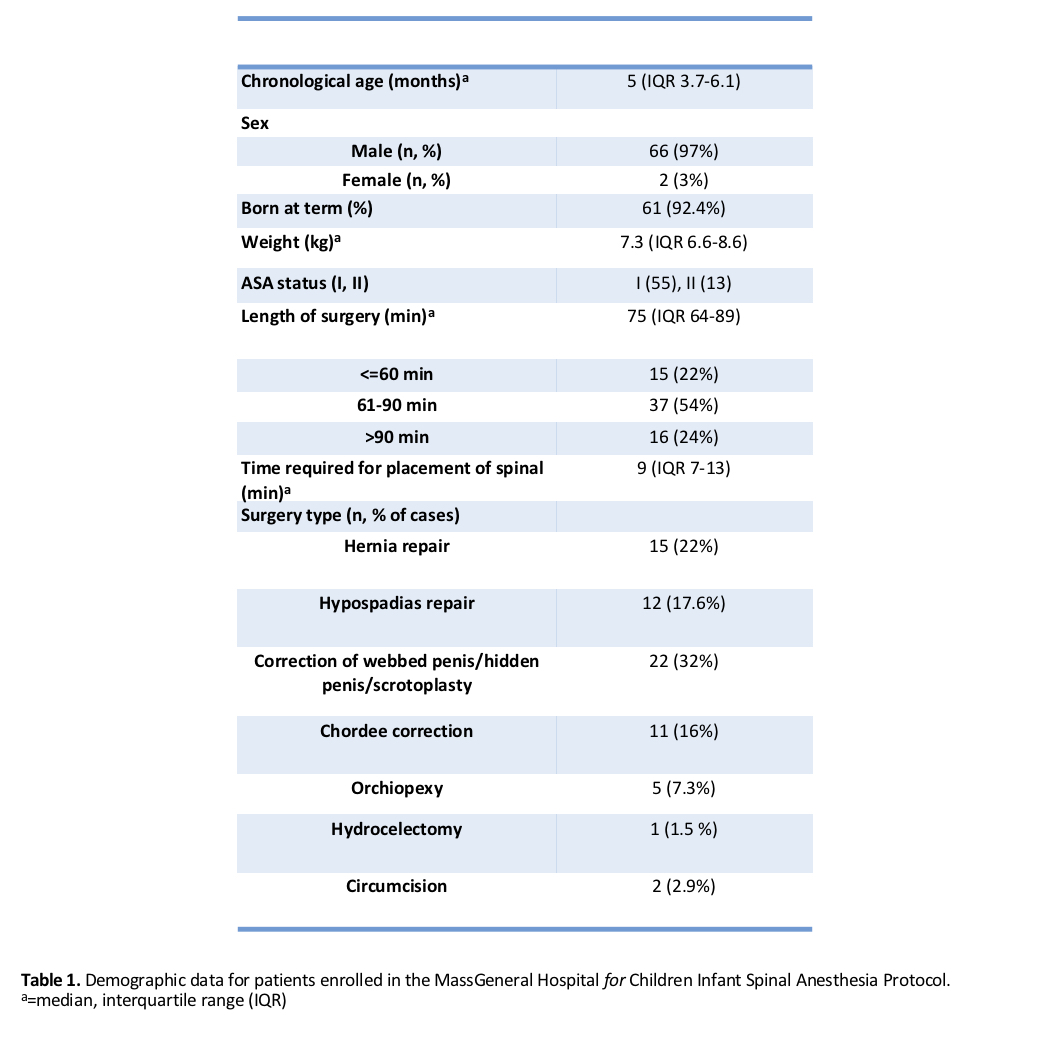
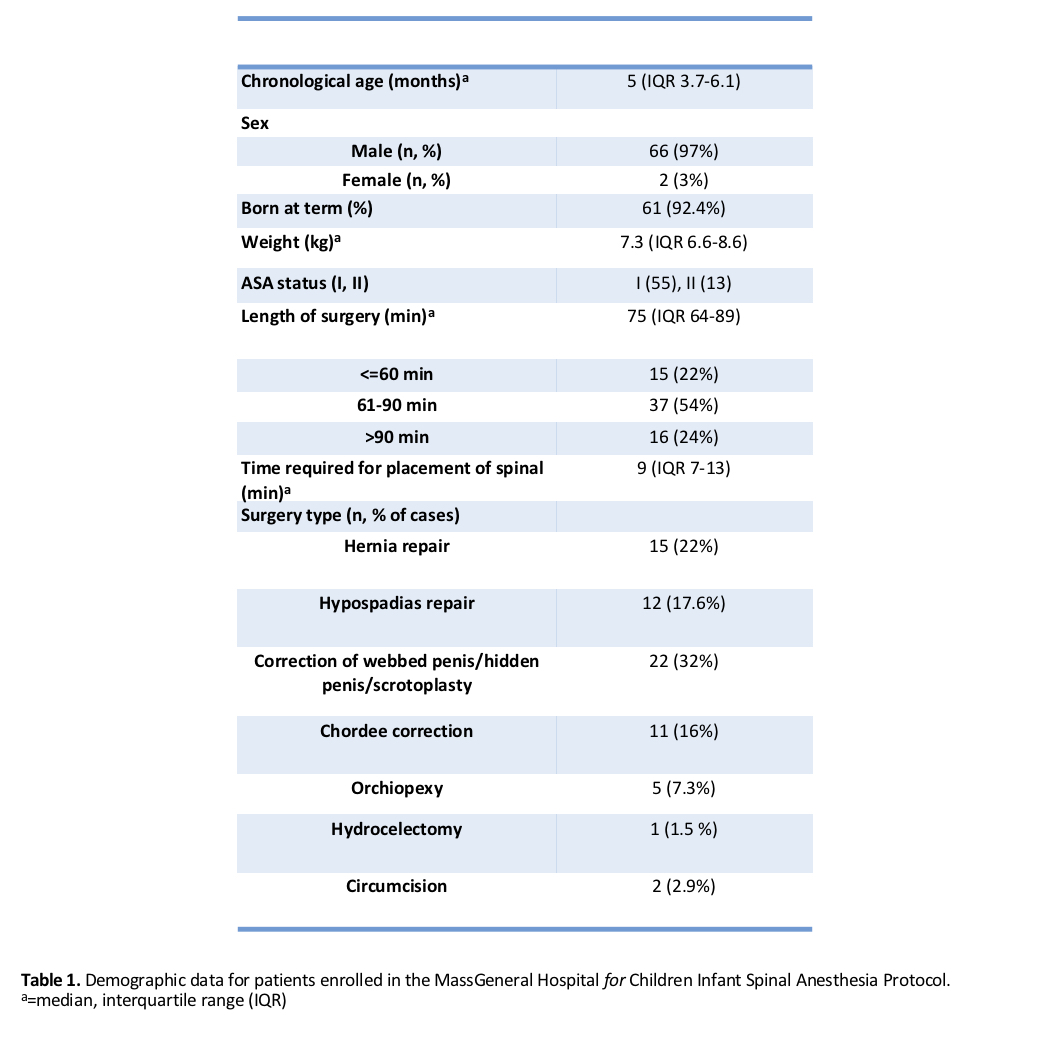
Results: A total of 68 patients were included (Table 1). Mean patient age was 5 months and mean weight was 7.3 kg. Average time for placement of SA was 10.4 ± 2.5 minutes. Clonidine was administered in 42/68 (61.8%), and combined spinal/caudal anesthesia was employed in 8/68 (11.8%). Operative time was > 60 minutes in 53 (78%). Of the 68 cases, 1 was converted to GA (1.5%) due to intolerance of laparoscopic insufflation. Adjunctive intravenous sedation was required in 14 cases. Average procedure time was significantly higher among cases performed with combined spinal/caudal catheter (139 vs 73 mins, p < 0.001). Intraoperative apnea occurred in 7 patients (5 received clonidine, 2 did not, p = 0.285), of whom 4 required manual stimulation while none required further intervention. There were no anesthetic events requiring post-operative management. All patients were brought awake and ready to feed to the PACU and discharged after feeding.
Conclusions: SA is a safe and effective alternative to GA in young infants undergoing outpatient genital surgery. SA reduces the need for invasive airway placement, improves OR efficiency, and shortens PACU time. Surgical time can be prolonged by use of adjuncts such as clonidine and combined spinal/caudal catheter.
Source of Funding: None
Methods: A prospective IRB-approved database for pediatric patients undergoing urologic surgery under SA was created. Typically, patients < 10 months and < 10 kg are selected for SA. EMLA cream is applied to the L3-L5 interspace for 30 minutes. Patients receive intrathecal plain 0.5% bupivacaine 1 mg/kg without additional sedatives. Clonidine 1 µg/ml is added to extend the duration of the block if the procedure is anticipated to last > 75 minutes. Patients are soothed with a sugar solution and pacifier. Patients receive a caudal block following the procedure for postoperative pain relief. Patient age, gestational age, weight, time to place spinal anesthetic, spinal medication(s) used, surgical procedure, procedure length and peri-anesthetic events were recorded.
Results: A total of 68 patients were included (Table 1). Mean patient age was 5 months and mean weight was 7.3 kg. Average time for placement of SA was 10.4 ± 2.5 minutes. Clonidine was administered in 42/68 (61.8%), and combined spinal/caudal anesthesia was employed in 8/68 (11.8%). Operative time was > 60 minutes in 53 (78%). Of the 68 cases, 1 was converted to GA (1.5%) due to intolerance of laparoscopic insufflation. Adjunctive intravenous sedation was required in 14 cases. Average procedure time was significantly higher among cases performed with combined spinal/caudal catheter (139 vs 73 mins, p < 0.001). Intraoperative apnea occurred in 7 patients (5 received clonidine, 2 did not, p = 0.285), of whom 4 required manual stimulation while none required further intervention. There were no anesthetic events requiring post-operative management. All patients were brought awake and ready to feed to the PACU and discharged after feeding.
Conclusions: SA is a safe and effective alternative to GA in young infants undergoing outpatient genital surgery. SA reduces the need for invasive airway placement, improves OR efficiency, and shortens PACU time. Surgical time can be prolonged by use of adjuncts such as clonidine and combined spinal/caudal catheter.
Source of Funding: None

.jpg)
.jpg)