Back
Poster, Podium & Video Sessions
Moderated Poster
MP08: Pediatric Urology: Penis & Scrotum
MP08-19: Factors Affecting Orchiopexy Guideline Adherence
Friday, May 13, 2022
10:30 AM – 11:45 AM
Location: Room 225
Andrea Balthazar*, Ted Lee, Tanya Logvinenko, Caleb Nelson, Hsin-Hsiao Scott Wang, Caleb Nelson, Boston, MA

Andrea K. Balthazar, MD
Boston Children's Hospital Department of Urology
Poster Presenter(s)
Introduction: Cryptorchidism affects 3%-5% of term males. AUA guidelines for evaluating and treating cryptorchidism recommend surgical repair before 18 months of age (MoA) in boys with unilateral or bilateral cryptorchidism. Our objective was to understand the factors associated with cryptorchidism guideline adherence.
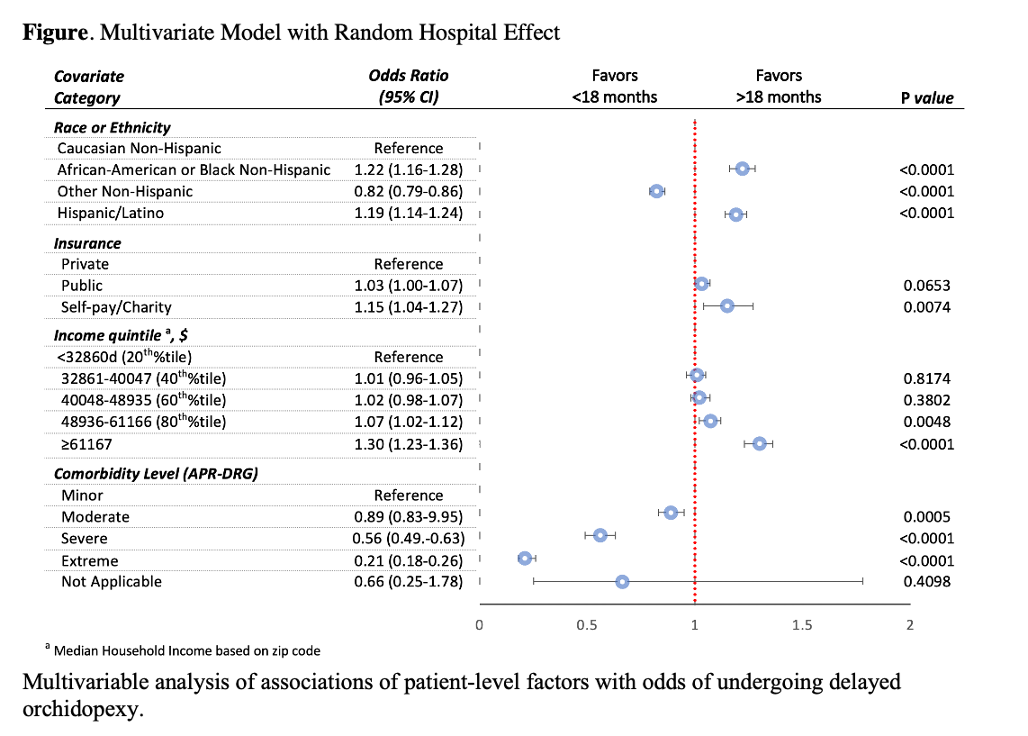
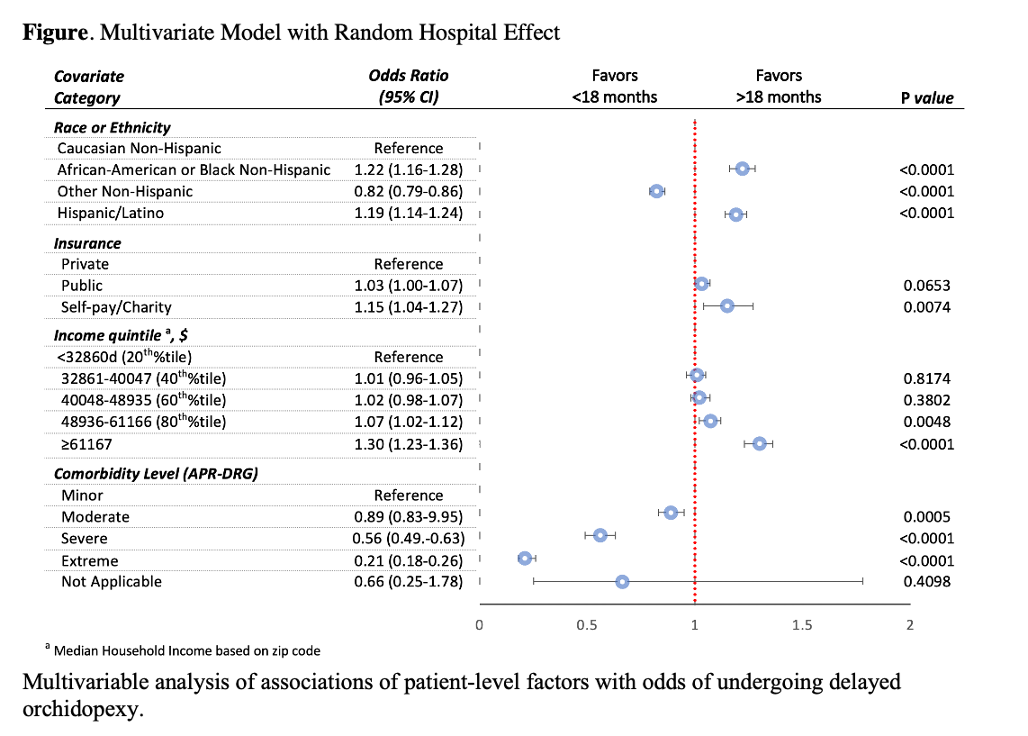
Methods: Pediatric Health Information System (PHIS) is a database of freestanding children’s hospitals. Using PHIS, we performed a multicenter retrospective study of boys ages 18 years and younger undergoing orchiopexy between 1/1/2009-12/31/2019. Categorized subjects by race/ethnicity(R/E) (Hispanic defined as any subject who identifies as Hispanic regardless of race), insurance type, income quintile, and presence of comorbid conditions. PHIS hospitals without outpatient surgery information were excluded. We fitted multivariate mixed-effects logistic regression models to evaluate the association of sociodemographic factors with the odds of undergoing surgery after 18 MoA (hospital-level as random effect). Multiple imputations were used for missing observations. Sensitivity analysis (SA) was performed for 18 and 24 MoA.
Results: 89114 cryptorchid males had orchiopexy between 2009-2019; 59093 (66.3%) surgeries occurred =18 MoA. 45303 (50.8%) were White, and 42213 (47.4%) had public insurance. Increased odds of orchiopexy after 18 MoA correlates with Black or Hispanic (P < 0.001), self-pay/charity (P=0.007), higher-income quintile (P <0.001), and lower comorbidity level (P <0.001). Black (OR=1.22; 95% CI, 1.16-1.28; P <0.001) and Hispanic (OR=1.19; 95% CI, 1.14-1.24; P <0.001) were at increased odds of delayed orchiopexy compared to Whites. We did not attribute the associations of R/E, insurance, or income with the outcome to single hospitals. The highest income compared to lowest was associated with increased odds of surgery after 18 MoA at 29/34 hospitals (85%). Compared to private insurance, public correlates with increased odds of surgical delay at 13/34 hospitals (38%). SA with 24 MoA with similar results.
Conclusions: Consistent with prior studies, orchiopexy remains delayed despite guidelines. In addition, Black, Hispanic, self-pay/charity, and lower comorbidity were significantly associated with delay. This highlights a need to refine provider education & outreach efforts to reduce disparities in care.
Source of Funding: 5T32DK060442
Methods: Pediatric Health Information System (PHIS) is a database of freestanding children’s hospitals. Using PHIS, we performed a multicenter retrospective study of boys ages 18 years and younger undergoing orchiopexy between 1/1/2009-12/31/2019. Categorized subjects by race/ethnicity(R/E) (Hispanic defined as any subject who identifies as Hispanic regardless of race), insurance type, income quintile, and presence of comorbid conditions. PHIS hospitals without outpatient surgery information were excluded. We fitted multivariate mixed-effects logistic regression models to evaluate the association of sociodemographic factors with the odds of undergoing surgery after 18 MoA (hospital-level as random effect). Multiple imputations were used for missing observations. Sensitivity analysis (SA) was performed for 18 and 24 MoA.
Results: 89114 cryptorchid males had orchiopexy between 2009-2019; 59093 (66.3%) surgeries occurred =18 MoA. 45303 (50.8%) were White, and 42213 (47.4%) had public insurance. Increased odds of orchiopexy after 18 MoA correlates with Black or Hispanic (P < 0.001), self-pay/charity (P=0.007), higher-income quintile (P <0.001), and lower comorbidity level (P <0.001). Black (OR=1.22; 95% CI, 1.16-1.28; P <0.001) and Hispanic (OR=1.19; 95% CI, 1.14-1.24; P <0.001) were at increased odds of delayed orchiopexy compared to Whites. We did not attribute the associations of R/E, insurance, or income with the outcome to single hospitals. The highest income compared to lowest was associated with increased odds of surgery after 18 MoA at 29/34 hospitals (85%). Compared to private insurance, public correlates with increased odds of surgical delay at 13/34 hospitals (38%). SA with 24 MoA with similar results.
Conclusions: Consistent with prior studies, orchiopexy remains delayed despite guidelines. In addition, Black, Hispanic, self-pay/charity, and lower comorbidity were significantly associated with delay. This highlights a need to refine provider education & outreach efforts to reduce disparities in care.
Source of Funding: 5T32DK060442

.jpg)
.jpg)