Back
Poster, Podium & Video Sessions
Moderated Poster
MP09: Prostate Cancer: Detection & Screening I
MP09-04: A Unique Comparison of Prostate Cancer Detection Rates between Transrectal versus Transperineal MRI-TRUS Fusion Prostate Biopsy among 794 Cases
Friday, May 13, 2022
10:30 AM – 11:45 AM
Location: Room 222
Renée Hogenhout*, Henk B. Luiting, Daniël F. Osses, Monique J. Roobol, Rotterdam, Netherlands

Renee Hogenhout, MSC
PhD candidate
Erasmus MC Cancer Institute
Poster Presenter(s)
Introduction: Currently, transperineal prostate biopsy (TPB) is preferred over transrectal biopsy (TRB) due to the lower risk of infectious complications. From an oncological point of view, prostate cancer (PCa) detection rates, when performed without prior MRI, are comparable between the transrectal (TRB) and transperineal (TPB) approach. Our aim was to compare the PCa detection rate between the two approaches when MRI-TRUS fusion biopsy is performed.
Methods: We prospectively included prostate biopsy-naïve men, men with prior negative biopsy, and men on active surveillance who had a suspicious lesion on MRI and underwent biopsy in Erasmus MC between Apr 2013 – Oct 2021. MRI-TRUS fusion biopsy was performed in all men: TRB until Dec 2019 and thereafter TPB, both under local anesthesia. With MRI-TRUS fusion biopsy, suspicious lesions on MRI are fused with real-time ultrasound (TRUS) as guidance for targeted biopsies. Detection rates of clinically significant (cs)PCa (i.e. Grade Group (GG) =2) between the two biopsy techniques were compared. For men on active surveillance, the endpoint was reclassification to a higher GG.
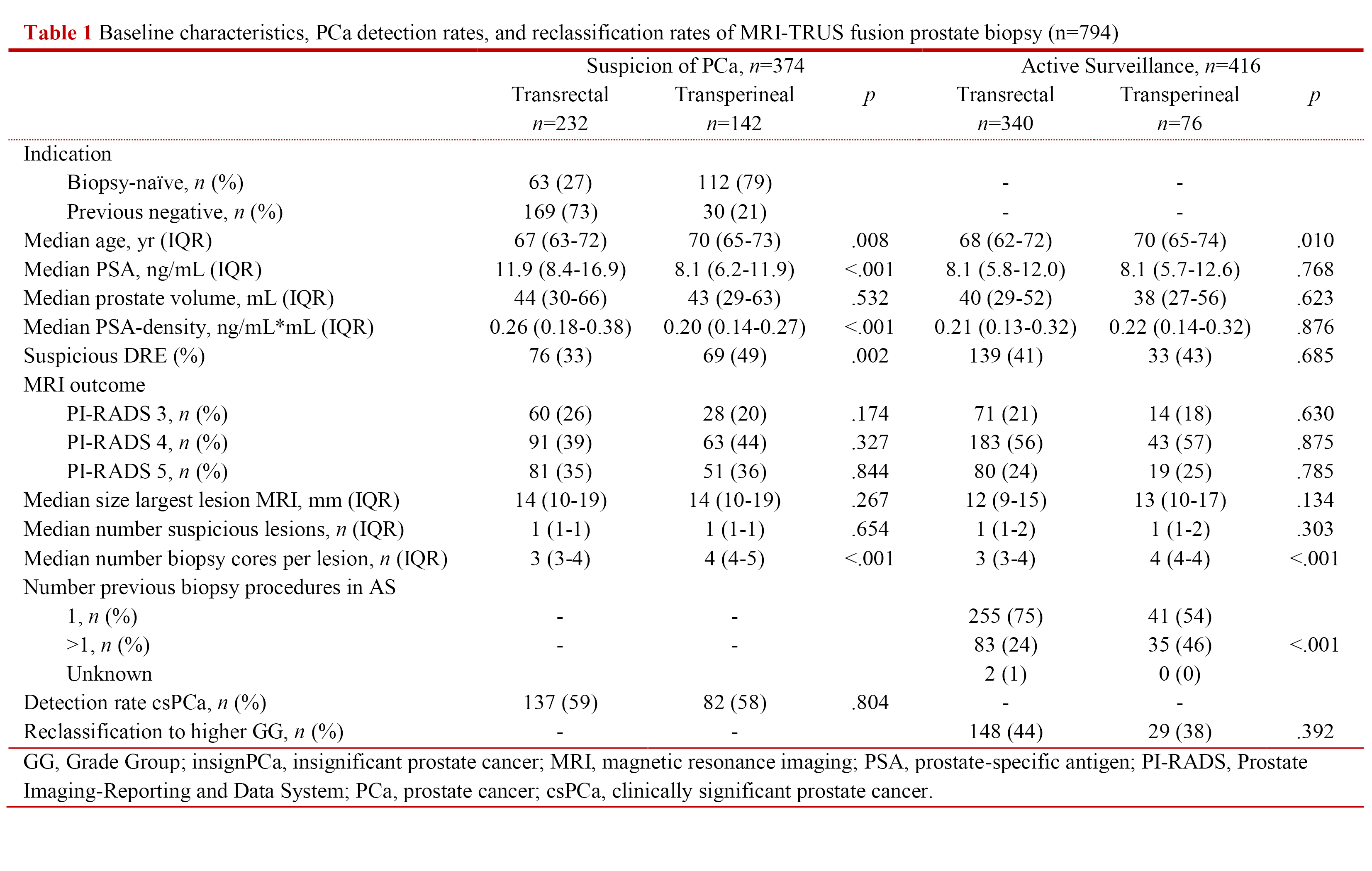
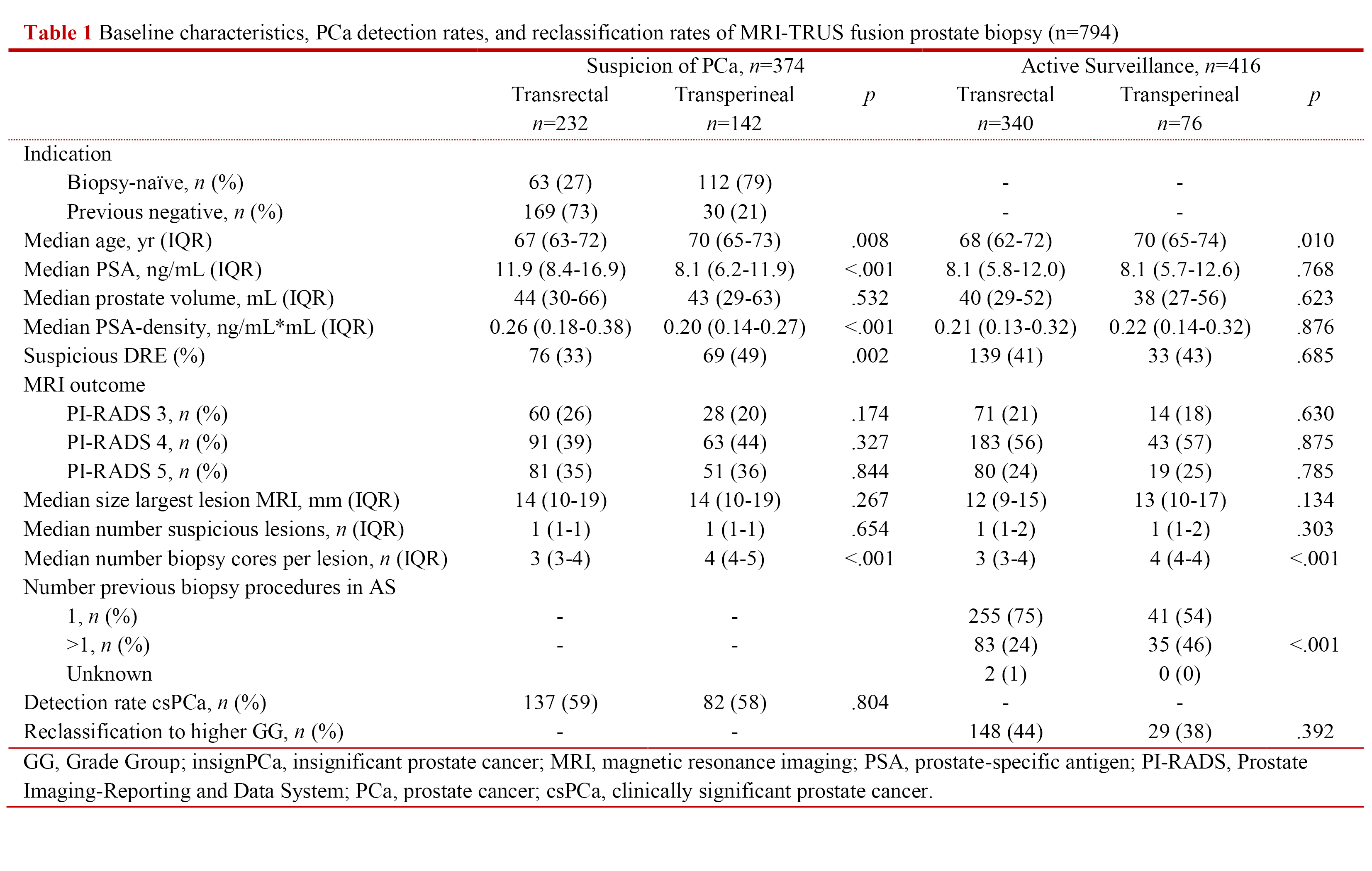
Results: In total, 794 prostate biopsy procedures were included for analysis of which 575 TRB and 219 TPB (Table 1). In men with suspicion of PCa, multivariable logistic regression analysis showed that the detection rate of csPCa for TPB was not significantly different from TRB (59% vs 58%; OR 1.00; p=0.987; 95% CI: 0.53-1.88) when corrected for age, PSA-density, DRE, PI-RADS, number of biopsy cores per lesion, and indication (i.e. biopsy-naïve, previous negative). In men on active surveillance reclassification to a higher GG did also not defer between the biopsy techniques (TPB 44% vs TRB 38%; OR 0.71; p=0.266; 95% CI: 0.39-1.30) when corrected for age, PSA-density, DRE, PI-RADS, number of biopsy cores per lesion, and number of previous biopsy procedures.
Conclusions: We performed a unique comparison of TRB and TPB in which both MRI-TRUS fusion biopsy was performed: detection rates for csPCa were comparable between the two approaches in men with suspicion of PCa. The same was found for reclassification in men on active surveillance. Therefore, TPB is a safe technique both in terms of infectious complications and cancer detection, also when MRI-TRUS fusion is used.
Source of Funding: None.
Methods: We prospectively included prostate biopsy-naïve men, men with prior negative biopsy, and men on active surveillance who had a suspicious lesion on MRI and underwent biopsy in Erasmus MC between Apr 2013 – Oct 2021. MRI-TRUS fusion biopsy was performed in all men: TRB until Dec 2019 and thereafter TPB, both under local anesthesia. With MRI-TRUS fusion biopsy, suspicious lesions on MRI are fused with real-time ultrasound (TRUS) as guidance for targeted biopsies. Detection rates of clinically significant (cs)PCa (i.e. Grade Group (GG) =2) between the two biopsy techniques were compared. For men on active surveillance, the endpoint was reclassification to a higher GG.
Results: In total, 794 prostate biopsy procedures were included for analysis of which 575 TRB and 219 TPB (Table 1). In men with suspicion of PCa, multivariable logistic regression analysis showed that the detection rate of csPCa for TPB was not significantly different from TRB (59% vs 58%; OR 1.00; p=0.987; 95% CI: 0.53-1.88) when corrected for age, PSA-density, DRE, PI-RADS, number of biopsy cores per lesion, and indication (i.e. biopsy-naïve, previous negative). In men on active surveillance reclassification to a higher GG did also not defer between the biopsy techniques (TPB 44% vs TRB 38%; OR 0.71; p=0.266; 95% CI: 0.39-1.30) when corrected for age, PSA-density, DRE, PI-RADS, number of biopsy cores per lesion, and number of previous biopsy procedures.
Conclusions: We performed a unique comparison of TRB and TPB in which both MRI-TRUS fusion biopsy was performed: detection rates for csPCa were comparable between the two approaches in men with suspicion of PCa. The same was found for reclassification in men on active surveillance. Therefore, TPB is a safe technique both in terms of infectious complications and cancer detection, also when MRI-TRUS fusion is used.
Source of Funding: None.

.jpg)
.jpg)