Back
Poster, Podium & Video Sessions
Moderated Poster
MP09: Prostate Cancer: Detection & Screening I
MP09-13: The value of [F-18]FlorastaminR Prostate Specific membranous antigen (PSMA) PET/CT at initial diagnosis of prostate cancer compared with multi-parametric magnetic resonance imaging (mpMRI)
Friday, May 13, 2022
10:30 AM – 11:45 AM
Location: Room 222
Hyeok Jae Kwon*, Chang Eil Yoon, Dongho Shin, Hyong Woo Moon, Yong Hyun Park, Woong Jin Bae, Hyuk Jin Cho, U-Syn Ha, Sung-Hoo Hong, Sae Woong Kim, Ji Youl Lee, Seoul, Korea, Republic of
- HK
Hyeok Jae Kwon, MD
The Catholic Univ. Of Korea Seoul St. Mary's Hospital
Poster Presenter(s)
Introduction: The prevalence rate of prostate cancer is increasing very fast and diagnosis tools become more important. Recently, multi-parametric magnetic resonance imaging (mpMRI) is the most commonly used for diagnosis, but it`s accuracy is not enough for high level of diagnostic power. Our study is to compare Prostate Specific membranous antigen (PSMA) PET/CT with mpMRI for detecting accuracy of clinically significant prostate cancer (csPCa: in this study, = gleason score 7 (3+4)) and detecting accuracy of cancer location correlation with biopsy result.
Methods: 82 patients, suspicious of prostate cancer (abnormal DRE Finding or PSA >3.0ng/ml), were recruited to this study. After [F-18] FlorastaminR PET/CT and mpMRI was filmed, saturation perineal biopsy (20 Core biopsy) was done. The positive criteria of MRI was more than PI-RAD score 3 but at [F-18] PSMA PET/CT, all the results were evaluated by the urologist who did prostate biopsy, referring to the standards (higher than background level, unrelated to physiological uptake or known pitfall). So, [F-18] PSMA PET/CT results were additionally classified as ambiguous. Therefore, we created four scenarios. Positive scenario(PS) was that all cases evaluated as ambiguous was included to positive group but Negative scenario(NS) was the opposite. Best scenario (BS) was that all the cases evaluated as ambiguous matched the biopsy results but Worst scenario (WS) was the opposite.
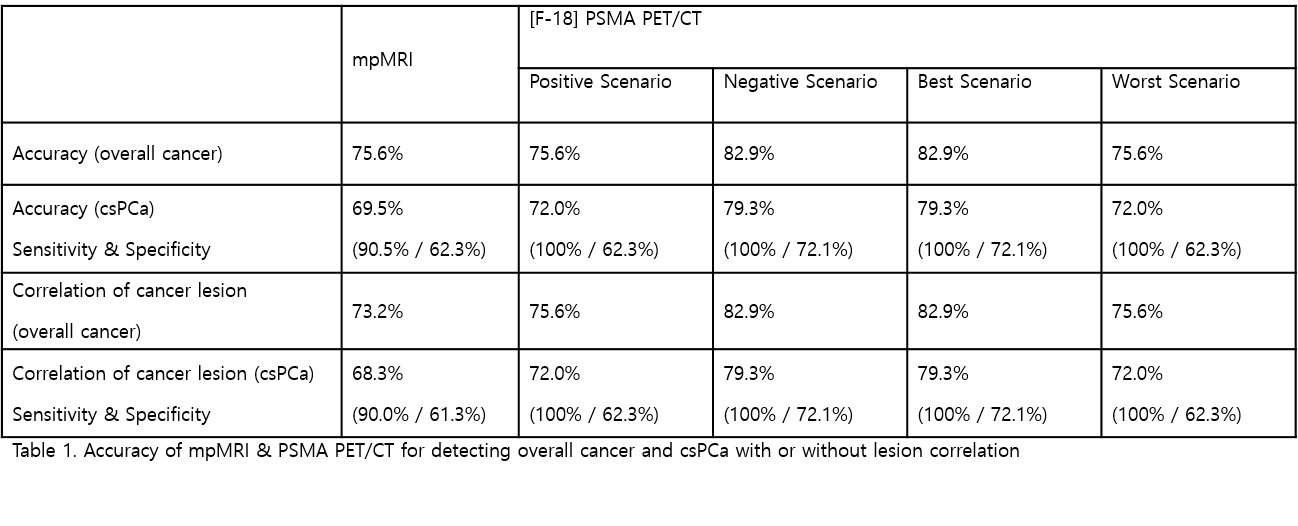
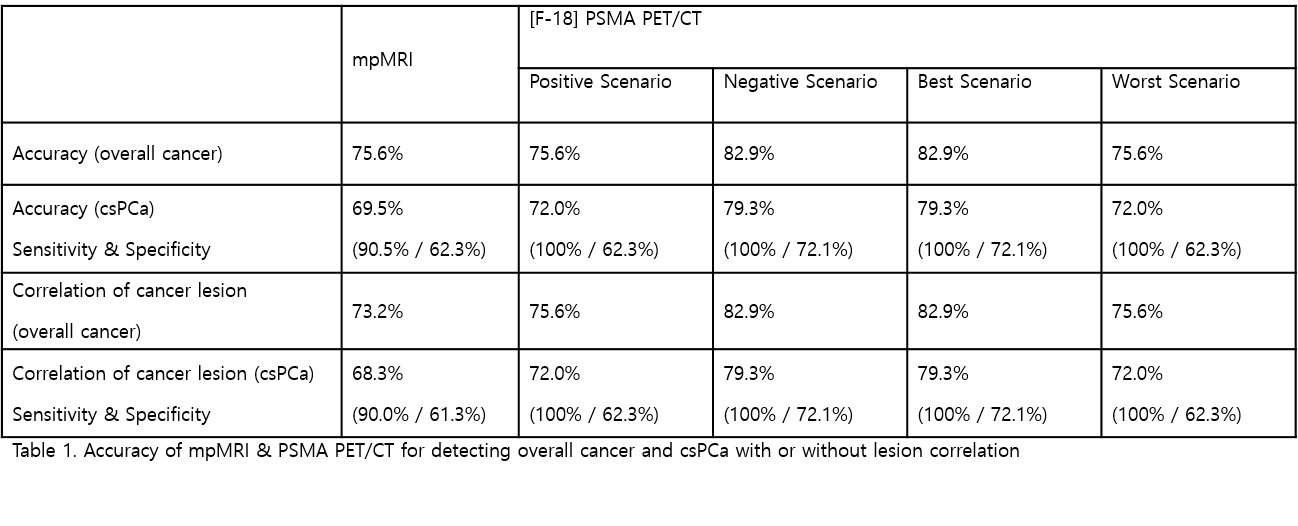
Results: Of the 82 patients, 27 were diagnosed with csPCa and mpMRI showed accuracy of 69.5%. PS & WS Showed the same accuracy of 72.0% but NS & BS showed the same accuracy of 79.3%. When we calculated cancer location detect accuracy, mpMRI showed accuracy of 68.3%. PS & WS showed the same accuracy of 72.0% but NS & BS showed the same accuracy of 79.3%. (Table 1)
Conclusions: This is the first study to use [F-18] Florastamin PET/CT for initial diagnostic tool of prostate cancer. The result shows that csPCa detection accuracy of PSMA PET/CT is higher than MRI, and location detection accuracy is also higher. There was no csPCa that both PSMA PET/CT and mpMRI couldn`t detect. So perineal biopsy for prostate cancer will be more accurate when mpMRI and [F-18] Florastamin PET/CT are used together for diagnosis tool.
Source of Funding: Seoul St. Mary’s Hospital, Korea
Methods: 82 patients, suspicious of prostate cancer (abnormal DRE Finding or PSA >3.0ng/ml), were recruited to this study. After [F-18] FlorastaminR PET/CT and mpMRI was filmed, saturation perineal biopsy (20 Core biopsy) was done. The positive criteria of MRI was more than PI-RAD score 3 but at [F-18] PSMA PET/CT, all the results were evaluated by the urologist who did prostate biopsy, referring to the standards (higher than background level, unrelated to physiological uptake or known pitfall). So, [F-18] PSMA PET/CT results were additionally classified as ambiguous. Therefore, we created four scenarios. Positive scenario(PS) was that all cases evaluated as ambiguous was included to positive group but Negative scenario(NS) was the opposite. Best scenario (BS) was that all the cases evaluated as ambiguous matched the biopsy results but Worst scenario (WS) was the opposite.
Results: Of the 82 patients, 27 were diagnosed with csPCa and mpMRI showed accuracy of 69.5%. PS & WS Showed the same accuracy of 72.0% but NS & BS showed the same accuracy of 79.3%. When we calculated cancer location detect accuracy, mpMRI showed accuracy of 68.3%. PS & WS showed the same accuracy of 72.0% but NS & BS showed the same accuracy of 79.3%. (Table 1)
Conclusions: This is the first study to use [F-18] Florastamin PET/CT for initial diagnostic tool of prostate cancer. The result shows that csPCa detection accuracy of PSMA PET/CT is higher than MRI, and location detection accuracy is also higher. There was no csPCa that both PSMA PET/CT and mpMRI couldn`t detect. So perineal biopsy for prostate cancer will be more accurate when mpMRI and [F-18] Florastamin PET/CT are used together for diagnosis tool.
Source of Funding: Seoul St. Mary’s Hospital, Korea

.jpg)
.jpg)